
Author: Dr. Joseph Tauro, MD
Knee arthritis is a widespread condition that affects millions globally, causing significant pain, stiffness, and reduced mobility. Preventing and effectively treating knee arthritis is essential for maintaining an active and healthy lifestyle. Dr. Joseph Tauro, a renowned board-certified orthopedic surgeon at Advanced Orthopedics and Sports Medicine Institute (AOSMI), shares his expert strategies on how to prevent and manage knee arthritis to help you stay active and pain-free.
Understanding Knee Arthritis
Knee arthritis occurs when the cartilage in the knee joint wears down, causing bones to rub against each other. This can lead to pain, swelling, and reduced joint function. The most common types of knee arthritis are:
1. Osteoarthritis:
A degenerative joint disease that occurs with aging and wear and tear.
2. Rheumatoid Arthritis:
An autoimmune disease that causes inflammation in the joints.
3. Post-Traumatic Arthritis:
Arthritis that develops after an injury to the knee.
Symptoms of Knee Arthritis
Recognizing the symptoms of knee arthritis early can help in managing the condition more effectively. Common symptoms include:
-
Pain:
Often worsens with activity and improves with rest.
-
Stiffness:
Particularly in the morning or after sitting for a long period.
-
Swelling:
Around the knee joint.
-
Reduced Mobility:
Difficulty bending or straightening the knee.
-
Creaking or Popping:
Sensations when moving the knee.

Preventing Knee Arthritis
While some risk factors for knee arthritis such as age and genetics cannot be controlled, there are several steps you can take to reduce your risk:
1. Maintain a Healthy Weight:
Excess weight puts additional stress on your knees. Losing weight can significantly reduce the risk of developing knee arthritis and can reduce your symptoms if you already have arthritis.
2. Stay Active:
Regular exercise helps to strengthen the muscles around the knee, providing better support and reducing the strain on the joint.
3. Protect Your Knees:
Use proper techniques when lifting heavy objects and avoid activities that put excessive strain on your knees.
4. Eat a Balanced Diet:
Nutrients such as vitamin D and calcium are essential for bone health. Anti-inflammatory foods like fish, nuts, and leafy greens can help reduce inflammation. You should try to avoid fried and highly processed foods.
5. Avoid Repetitive Stress:
Take breaks and use ergonomic tools to minimize repetitive strain on your knees.
Treating Knee Arthritis
If you are already experiencing symptoms of knee arthritis, there are several treatment options available to help manage the condition and improve your quality of life:
1. Medications:
-
-
- Pain Relievers: Over-the-counter medications like acetaminophen or NSAIDs(such as ibuprofen or naproxen) can help reduce pain and inflammation.
- Corticosteroid Injections: These can provide temporary relief from more severe and acute pain and swelling. Repetitive steroid injections can actually cause further joint damage and so are not recommended.
- Viscosupplimentation injections: Commonly referred to as gel shots, these can also reduce pain. They usually take a bit longer to take effect but can last longer. They do not cause further joint damage if used no more than once every 6 months.
- PRP/Platelet Rich Plasma injections: This is a biologic solution where we draw your own blood and process it to isolate plasma high in platelets and anti inflammatory proteins. This is then injected back into your knee. This is an effective and scientifically proven therapy but is not usually covered by insurance.
-
2. Physical Therapy:
A physical therapist can design a personalized exercise program to strengthen the muscles around the knee and improve flexibility. Pain and swelling usually can be reduced by modalities such as stims and ice compression.
3. Knee supports and Braces:
Using braces can help reduce the pressure on your knees, especially if the arthritis is confined to just the inner or outer part of the knee.
4. Lifestyle Modifications:
Adopting a healthy diet, staying active, and maintaining a healthy weight are crucial for managing knee arthritis.
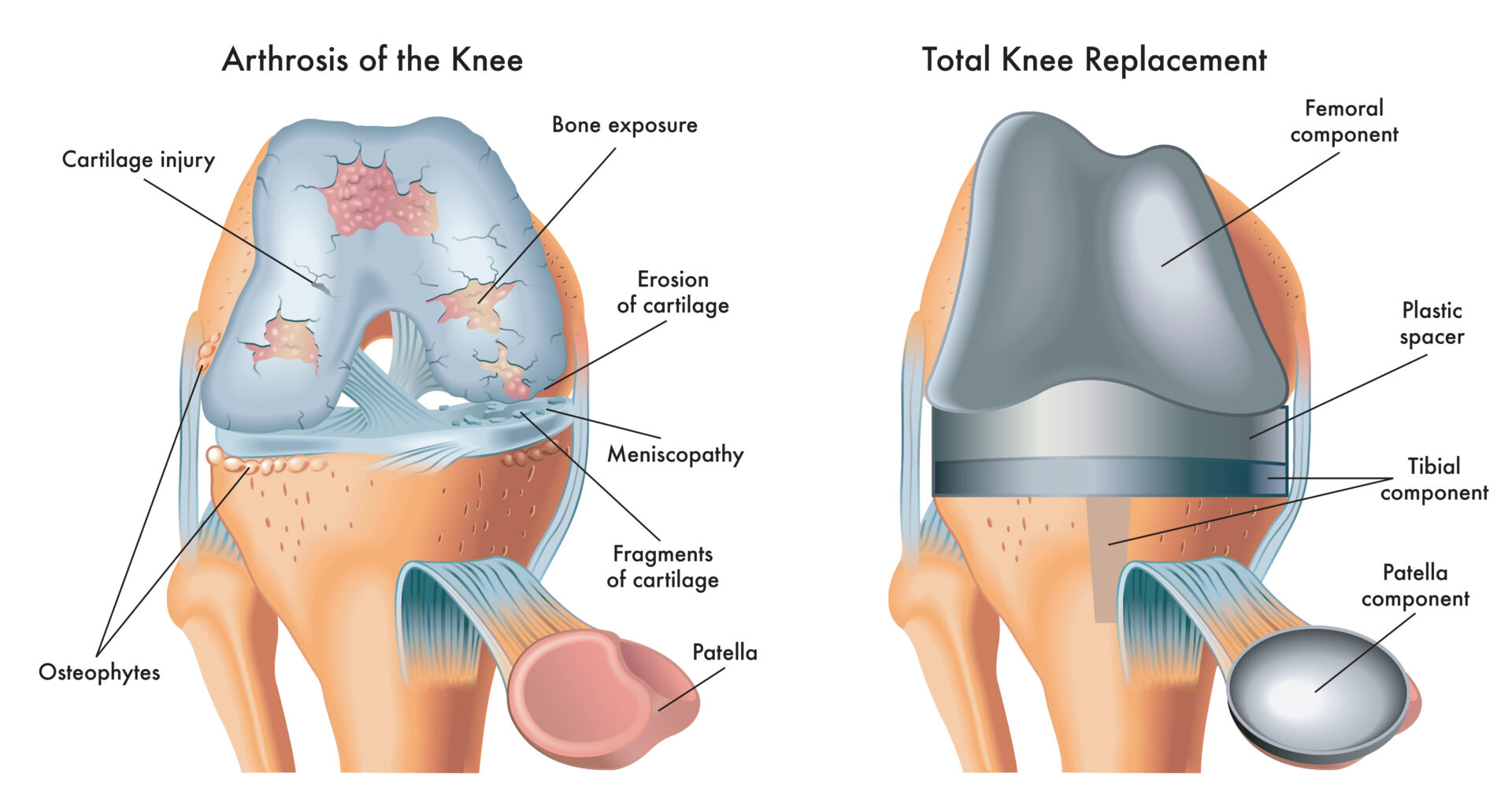
5. Surgical Options:
In severe cases, surgical interventions such as knee arthroscopy, osteotomy, or total knee replacement may be necessary. In younger patients with a localized area of joint surface damage, cartilage grafting can be very effective. Dr. Tauro specializes in these advanced surgical techniques to provide the best outcomes for his patients.
6. Knee supports and Braces:
Using braces can help reduce the pressure on your knees, especially if the arthritis is confined to just the inner or outer part of the knee.
7. Lifestyle Modifications:
Adopting a healthy diet, staying active, and maintaining a healthy weight are crucial for managing knee arthritis.
8. Surgical Options:
In severe cases, surgical interventions such as knee arthroscopy, osteotomy, or total knee replacement may be necessary. In younger patients with a localized area of joint surface damage, cartilage grafting can be very effective. Dr. Tauro specializes in these advanced surgical techniques to provide the best outcomes for his patients.
Conclusion
Knee arthritis can be a challenging condition, but with the right prevention and treatment strategies, you can manage your symptoms and maintain a high quality of life. Dr. Joseph Tauro and the team at AOSMI are dedicated to providing personalized care and advanced treatment options for knee arthritis. If you’re experiencing knee pain or stiffness, don’t hesitate to seek professional help.
Don’t let knee pain hold you back any longer. Take control of your knee health today by scheduling a consultation with Dr. Joseph Tauro at AOSMI. Visit our website, call us at 732.907.8798 to book your appointment. We’re here to help you live a pain-free, active life!
About the Author:
Dr. Joseph Tauro is board-certified by the American Board of Orthopedic Surgeons and is a nationally recognized expert in the treatment of shoulder, sports, and degenerative joint disorders. Dr. Tauro’s position at Rutgers Medical School and his role as a national lecturer on the latest orthopedic techniques assure patients of receiving the finest care available. Patients with complex problems are often referred to Dr. Tauro from across the United States.
Undergoing a total knee replacement can be a transformative experience, offering relief from chronic pain and improved mobility. However, the road to recovery involves careful planning and adherence to rehabilitation strategies to ensure the best outcomes. Here are some essential tips to help you navigate life after your knee replacement surgery.
Follow Your Rehabilitation Plan
One of the most crucial aspects of recovery is following your prescribed rehabilitation plan. Physical therapy plays a key role in regaining strength, flexibility, and range of motion in your new knee. Your therapist will guide you through exercises designed to improve joint function and reduce stiffness. Consistency is key, so make sure to adhere to the exercise regimen and attend all scheduled therapy sessions.
Manage Pain and Swelling
Post-surgical pain and swelling are common, but effective management can significantly enhance your comfort and recovery speed. Use prescribed pain medications as directed and apply ice packs to reduce swelling. Elevating your leg and following any additional pain management techniques suggested by your healthcare provider will also aid in a smoother recovery.
Gradual Return to Activities
While it’s important to stay active, it’s equally important to ease back into your daily activities gradually. Avoid high-impact exercises and strenuous activities until your knee has healed sufficiently. Your healthcare provider will provide guidance on when you can safely resume various activities, including driving, walking, and other physical tasks.
Monitor for Complications
Be vigilant for signs of complications, such as excessive swelling, redness, or unusual pain. Contact your healthcare provider if you experience any concerning symptoms or if your recovery isn’t progressing as expected.
Stay Positive and Patient
Recovery from total knee replacement is a gradual process, and maintaining a positive mindset can greatly impact your overall experience. Be patient with yourself and celebrate small victories along the way.
Turn to AOSMI for Support
At AOSMI, our team is dedicated to supporting you through every stage of your recovery journey. From personalized rehabilitation plans to expert care, we’re here to help you achieve a successful recovery. Reach out to us today to learn more about our services and how we can assist you in getting back to your best self.
We are thrilled to announce that several esteemed physicians from Advanced Orthopedics and Sports Medicine Institute (AOSMI) have been recognized as NJ Top Docs for 2024. This prestigious honor underscores our commitment to providing exceptional orthopedic care and advanced treatment options for our patients in New Jersey.
About the Top Docs Awards
The Top Docs awards are based on a rigorous selection process. Nominees complete a comprehensive qualification questionnaire covering their education, training, years in practice, continuing education, licensing, publications, charitable work, professional appointments, and achievements. Each component is verified to ensure that nominees meet the high standards set by the Top Docs organization. Board certification is required for applicable specialties, and nominees must also undergo a thorough review of malpractice and licensing records to confirm there are no serious issues. Patient reviews are collected and compiled to provide a comprehensive assessment of each nominee’s performance.
Join us in celebrating the remarkable accomplishments of the following Top Docs nominees:

Michael J. Greller, MD, MBA, CPE, FAAOS
Dr. Michael J. Greller is a Board-certified orthopedic surgeon specializing in sports medicine and joint preservation. His comprehensive approach to patient care, combined with his administrative expertise, has established him as a leader in orthopedic surgery. Dr. Greller’s commitment to excellence is evident in both his clinical and organizational contributions to AOSMI.

Ali Valimahomed, MD, FAAPMR
Dr. Ali Valimahomed is a dual Board-certified specialist in Pain Medicine and Physical Medicine & Rehabilitation. His expertise lies in comprehensive pain management and restoring function to patients suffering from chronic pain conditions. Dr. Valimahomed’s holistic approach and dedication to improving patients’ quality of life make him a standout in his field.

Alison Dewaters, DPM, FACFAS
Dr. Alison Dewaters is a Board-certified podiatric surgeon with a focus on reconstructive foot and ankle surgery. As a Fellow of the American College of Foot and Ankle Surgeons, Dr. Dewaters is renowned for her surgical precision and compassionate patient care, ensuring optimal outcomes for her patients.

Arth Patel, MD, MPH
Dr. Arth Patel is a Board-certified Primary Care Sports Medicine physician with a background in Family Medicine. He is dedicated to the non-operative management of musculoskeletal injuries, promoting wellness and injury prevention. Dr. Patel’s patient-centered approach and emphasis on holistic care have earned him a well-deserved place among NJ’s top doctors.

Eric Buxbaum, DO, FAAOS
Dr. Eric Buxbaum is a Board-certified orthopedic surgeon with expertise in hip and knee replacement surgery. His focus on advanced surgical techniques and patient-centric care has made him a trusted name in joint health. Dr. Buxbaum’s approach combines precision with compassion, ensuring his patients receive the best possible care.

Joseph Tauro, MD
Dr. Joseph Tauro is a nationally recognized expert in shoulder, sports and degenerative joint disorders, known for his pioneering techniques in arthroscopic surgery. As a Board-certified Orthopedic Surgeon, Dr. Tauro’s contributions to the field have set new standards in patient care and surgical excellence. His innovative approach ensures that patients receive the most advanced and effective treatments available.

Stacey Gallacher, MD, FAAOS
Dr. Stacey Gallacher is a dual Board-certified orthopedic surgeon specializing in shoulder and elbow surgery and trauma care. Her precise surgical skills and compassionate patient care have made her a trusted specialist in her field. Dr. Gallacher’s dedication to improving patient outcomes through both surgical and non-surgical interventions is commendable.

Gerardo Goldberger, DO, FAOAO
Dr. Gerardo Goldberger is a Board-Certified orthopedic surgeon and Fellow of the American Osteopathic Academy of Orthopedics. His specialization in sports medicine and arthroscopic surgery allows him to effectively treat a wide range of athletic injuries. Dr. Goldberger’s dedication to his patients and innovative treatment methods make him a top choice for orthopedic care.

David Kirschenbaum, MD
Dr. David Kirschenbaum is an hand and upper extremity Fellowship-Trained orthopedic surgeon. His extensive experience and commitment to cutting-edge techniques provide patients with innovative solutions for their orthopedic needs. Dr. Kirschenbaum’s dedication to excellence is reflected in his high patient satisfaction and successful surgical outcomes.

At AOSMI, we are incredibly proud of our doctors’ achievements and their unwavering commitment to providing the highest quality of orthopedic care. Being named NJ Top Docs is a testament to their expertise, compassion, and dedication to patient well-being. We extend our heartfelt congratulations to each of these outstanding physicians and look forward to their continued success in advancing orthopedic and sports medicine.
For more information or to schedule an appointment with any of our top doctors, please contact our office at (732) 335-6727 and schedule an appointment online. Together, we can achieve better health and a higher quality of life.
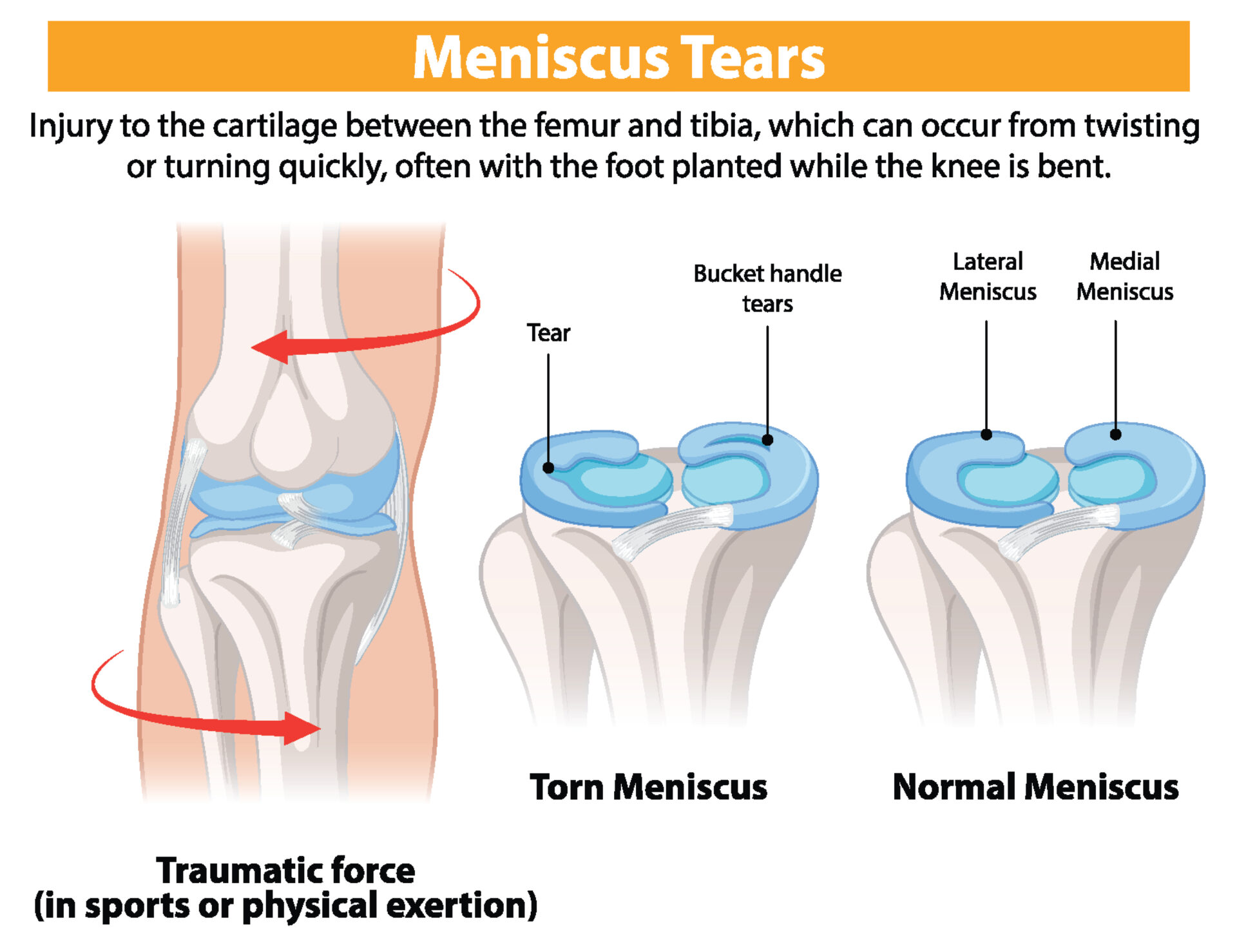
Knee meniscus injuries and ACL (Anterior Cruciate Ligament) injuries are common knee problems, especially among athletes. These injuries can cause pain, swelling, and instability in the knee. This guide will help you understand knee meniscus and ACL surgeries, including pre-surgery preparation, what to expect on the day of surgery, and post-surgery recovery.
About the Author: Joseph Tauro, MD, a Board-Certified orthopedic surgeon, is nationally recognized for his expertise in treating shoulder, sports, and degenerative joint disorders. As a professor at Rutgers Medical School and a Master Instructor for the Arthroscopy Association of North America (AANA), he leads the field in developing new techniques for minimally invasive joint replacement, arthroscopic shoulder surgery, and Augmented Reality surgical training. Patients from across the U.S. are referred to Dr. Tauro for his specialized care. Request an appointment with Dr. Tauro today to experience expert orthopedic care first-hand!
Pre-Surgery Guidelines for Knee Meniscus and ACL Surgery
What You Should Do Before Knee Surgery:
Consultation with Dr. Tauro:
- Have a thorough discussion with Dr. Tauro about the procedure, risks, and benefits of knee meniscus and ACL surgery.
Medical Clearance and Preparation:
- Most younger patients with no medical problems do not require medical clearance but if you are older and have a medical condition you may need to obtain medical clearance from your primary care physician.
- Review all medications with your doctor. You may need to stop certain medications, like blood thinners, a few days before surgery.
Physical and Home Preparation:
- Engage in pre-surgery physical therapy or a home therapy program if recommended to strengthen the knee muscles and restore range of motion before meniscus or ACL surgery.
- Arrange your home to accommodate your post-surgery needs. This might include setting up a comfortable resting area and ensuring easy access to necessities. You will feel more comfortable elevating your leg for sleep during the initial recovery phase after knee surgery.
What You Shouldn’t Do Before Knee Surgery:
Eating and Drinking:
- Do not eat or drink anything after midnight before your knee surgery day. This includes chewing gum, which can produce excessive saliva in your stomach.
Smoking and Alcohol:
- Avoid smoking as it can impair healing and increase the risk of complications.
- Do not consume alcohol at least 24 hours before knee surgery.

Day of Knee Meniscus and ACL Surgery
What to Do on the Day of Surgery:
Arrive on Time:
- Arrive at the hospital or surgical center at the scheduled time. The surgery center will call you with that time generally the day before your knee surgery.
Wear Comfortable Clothing:
- Wear loose, comfortable clothing that is easy to remove and put on.
Bring Essentials:
- Bring necessary documents and a list of medications.
What to Expect on the Day of Surgery:
Pre-Operative Preparation:
- You will undergo pre-operative preparations, including vital sign checks and anesthesia administration. For larger procedures such as an ACL reconstruction, anesthesia will usually include a regional block to numb the knee in addition to general anesthesia.
Surgery Duration:
- The procedure typically takes 1-2 hours, but this can vary depending on the extent of the meniscus or ACL repair.
Post-Operative Recovery:
- After surgery, you will be monitored in a recovery area until the anesthesia wears off.
Post-Operative Care and Recovery After Knee Meniscus and ACL Surgery
Immediate Post-Op Care:
Pain Management:
- Expect some pain and discomfort, which will be managed with prescribed medications. With the regional block, there is usually minimal pain initially, which can be managed with Tylenol and ibuprofen afterward.
Brace and Crutch Usage:
- For ACL surgery and meniscal repairs (as opposed to a simple partial removal of the meniscus), your knee will be immobilized in a brace, and you will need crutches to assist with walking after knee surgery.
Follow-Up Appointments:
- Schedule follow-up appointments with your surgeon, usually 1 week post-surgery. You can pre-schedule this appointment in our office before your knee surgery.

Phases of Recovery After Knee Meniscus and ACL Surgery:
Phase 1 (0-2 Weeks): Protection and Initial Healing
- Wear the brace as directed.
- Engage in range-of-motion exercises as prescribed by Dr. Tauro and your physical therapist.
- Avoid weight-bearing activities for meniscal repairs. ACL reconstructions and simple partial meniscectomies can bear weight as tolerated. Crutches are still required if you had an ACL surgery. Keep the knee elevated to reduce swelling.
Phase 2 (2-6 Weeks): Controlled Motion
- Gradually begin controlled motion exercises under the guidance of your physical therapist.
- Focus on restoring the range of motion without straining the knee. Isometric strengthening may also be recommended by Dr. Tauro and your therapist.
Phase 3 (6-12 Weeks): Strengthening
- Incorporate strengthening exercises for the knee and surrounding muscles.
- Continue to avoid heavy lifting or activities that place excessive strain on the knee.
Phase 4 (3-6 Months): Functional Training
- Progress to functional and sports-specific training as tolerated.
- Aim to return to normal activities and sports gradually, following Dr. Tauro’s and your physical therapist’s advice.
Full Recovery After Knee Meniscus and ACL Surgery:
Time Frame:
- Full recovery can take anywhere from 6 months to a year, depending on the extent of the repair and your adherence to the rehabilitation program. Most patients can return to activities like running and sports at 6-9 months post-op.
Rehabilitation:
- Consistent and dedicated rehabilitation is crucial for a successful outcome. Attend all therapy sessions and follow your doctor’s and your physical therapist’s instructions diligently.

Frequently Asked Questions (FAQs):
How long will I need to wear the brace after knee surgery?
- Typically, you will need to wear the brace for 4-6 weeks to protect the repair.
When can I return to work after knee meniscus or ACL surgery?
- This depends on your job and the extent of your surgery. Desk jobs may allow a return within a week or 2. More physical jobs may require several months.
Will I regain full range of motion after knee surgery?
- With proper rehabilitation, most patients regain normal or near normal motion, though individual results can vary.
Knee meniscus and ACL surgeries are highly effective procedures for treating knee injuries. By following the pre-surgery guidelines, preparing adequately, and adhering to the post-operative care and rehabilitation phases, you can achieve a successful recovery and regain full function of your knee. Always communicate with Dr. Tauro and our team of orthopedic experts at AOSMI if you have any concerns during your recovery journey. If you are experiencing knee pain, are considering knee meniscus surgery or ACL surgery, and would like a consultation, schedule an appointment with Dr. Tauro today!
Total knee replacement surgery is a common surgical procedure for individuals suffering from severe knee arthritis or injury. This surgery involves resurfacing the damaged knee joint with an artificial implant to relieve pain and restore function. This comprehensive guide will help you understand total knee replacement surgery, including pre-surgery preparation, what to expect on the day of surgery, and post-surgery recovery.
About the Author: Joseph Tauro, MD, a Board-Certified orthopedic surgeon, is nationally recognized for his expertise in treating shoulder, sports, and degenerative joint disorders. As a professor at Rutgers Medical School and a Master Instructor for the Arthroscopy Association of North America (AANA), he leads the field in developing new techniques for minimally invasive joint replacement, arthroscopic shoulder surgery, and Augmented Reality surgical training. Patients from across the U.S. are referred to Dr. Tauro for his specialized care. Request an appointment with Dr. Tauro today to experience expert orthopedic care first-hand!
Pre-Surgery Guidelines for Total Knee Replacement
What You Should Do Before Knee Replacement Surgery:
Consultation with Dr. Tauro:
- Have a thorough discussion with Dr. Tauro about the procedure, risks, and benefits of total knee replacement surgery.
- Dr. Tauro uses pre-operative computerized planning for almost all of the knee replacements he performs. This will involve the production of a custom guide to be used during your surgery. This greatly improves the accuracy of your surgery. You will need to go for a specialized MRI scan of your knee at least 6 weeks before your surgery to allow the use of this technology.
Medical Clearance and Preparation:
- Obtain medical clearance from your primary care physician if required.
- Review all medications with your doctor. You may need to stop certain medications, like blood thinners, a few days before surgery.
Physical and Home Preparation:
- Engage in pre-surgery physical therapy or a home therapy program if recommended to strengthen the knee muscles before knee replacement surgery.
- Arrange your home to accommodate your post-surgery needs. This might include setting up a comfortable resting area and ensuring easy access to necessities. You will need a walker or crutches for assistance after surgery.
What You Shouldn’t Do Before Knee Replacement Surgery:
Eating and Drinking:
- Do not eat or drink anything after midnight before your knee surgery day. This includes chewing gum, which can produce excessive saliva in your stomach.
Smoking and Alcohol:
- Avoid smoking as it can impair healing and increase the risk of complications.
- Do not consume alcohol at least 24 hours before knee replacement surgery.

Day of Total Knee Replacement Surgery
What to Do on the Day of Surgery:
Arrive on Time:
- Arrive at the hospital or surgical center at the scheduled time. The hospital or surgery center will call you with that time generally the day before your knee replacement surgery.
Wear Comfortable Clothing:
- Wear loose, comfortable clothing that is easy to remove and put on.
Bring Essentials:
- Bring necessary documents and a list of medications.
What to Expect on the Day of Surgery:
Pre-Operative Preparation:
- You will undergo pre-operative preparations, including vital sign checks and anesthesia administration. Anesthesia will usually include a regional block to numb the knee and spinal anesthesia.
Surgery Duration:
- The procedure typically takes 1-2 hours, but this can vary depending on the complexity of the knee replacement surgery.
Post-Operative Recovery:
- After surgery, you will be monitored in a recovery area until the anesthesia wears off.
Post-Operative Care and Recovery After Total Knee Replacement
Immediate Post-Op Care:
- Almost all knee replacements are considered outpatient procedures. You may go home the same day or we may keep you overnight if your operation was done in the hospital. Regardless, we will have you out of bed and in a chair the day of surgery and walking with a walker or crutches the same day or the morning after the surgery.
- We DO NOT send patients to inpatient rehabilitation facilities as we feel infection rates are higher and care is inconsistent. You are much better off at home in a clean, comfortable and familiar environment.
- You will need to make sure a friend or family member is with you for the first 2 days after discharge.
- We will make arrangements for physical therapy in your home for the first week or 2 after surgery. You will be given a prescription for outpatient therapy after your first visits with us 1 week after your surgery.
Prevention of Blood Clots:
- Please take an 81mg “baby” aspirin twice a day for three weeks after your surgery.
- If you are on stronger blood thinners (such as Elaquis or Xarelto) you should restart them the day after surgery.
Pain Management:
- Expect some pain and discomfort, which will be managed with prescribed medications. With the regional block, there is usually minimal pain initially, which can be managed with Tylenol and ibuprofen afterward. When the block wears off a few days after surgery, pain may increase and you may need stronger pain medication which we will prescribe. Make sure the hospital or surgery center has accurate information about your pharmacy.
Brace and Crutch Usage:
- You will likely need crutches or a walker to assist with walking after knee replacement surgery. Weight bearing is usually permitted immediately and progression to a cane and ultimately no assist will take place as soon as your comfort and stability is achieved.
Follow-Up Appointments:
- Schedule follow-up appointments with your surgeon, 1 week post-surgery. You should pre-schedule this appointment in our office before your knee replacement surgery.

Phases of Recovery After Total Knee Replacement Surgery:
Phase 1 (0-2 Weeks): Protection and Initial Healing
- Use crutches or a walker as directed.
- Engage in range-of-motion exercises as prescribed by Dr. Tauro and your physical therapist.
- Full weight bearing is usually permitted. the knee elevated to reduce swelling.
Phase 2 (2-6 Weeks): Controlled Motion
- Gradually increase controlled motion exercises under the guidance of your physical therapist.
- Isometric exercises and some light strengthening will be started by your physical therapist
- Focus on restoring the range of motion without straining the knee.
Phase 3 (6-12 Weeks): Strengthening
- Incorporate progressive strengthening exercises for the knee and surrounding muscles.
- Continue to avoid heavy lifting or activities that place excessive strain on the knee.
Phase 4 (3-6 Months): Functional Training
- Progress to functional and everyday activities as tolerated.
- Aim to return to normal activities gradually, following your therapist’s advice.
Full Recovery After Total Knee Replacement Surgery:
Time Frame:
- Full recovery can take anywhere from 4-6 months to a year, depending on the extent of the surgery and your adherence to the rehabilitation program. Most patients can return to activities like walking and light exercise at 6-12 weeks post-op.
Rehabilitation:
- Consistent and dedicated rehabilitation is crucial for a successful outcome. Attend all therapy sessions and follow your doctor’s and therapist’s instructions diligently.

Frequently Asked Questions (FAQs):
How long will I need to use crutches or a walker after knee replacement surgery?
- Typically, you will need to use crutches, a walker or a cane for 4-6 weeks to support your knee.
When can I return to work after total knee replacement surgery?
- This depends on your job and the extent of your surgery. Desk jobs may allow a return within a few weeks, while more physical jobs may require several months.
Will I regain full range of motion after knee replacement surgery?
- With proper rehabilitation, most patients regain a significant range of motion, though individual results can vary.
Strengthen your Knees with Total Knee Replacement Surgery at AOSMI in New Jersey!
Total knee replacement surgery is a highly effective procedure for treating severe knee arthritis and injury. By following the pre-surgery guidelines, preparing adequately, and adhering to the post-operative care and rehabilitation phases, you can achieve a successful recovery and regain full function of your knee. Always communicate with Dr. Tauro and our team of orthopedic experts at AOSMI if you have any concerns during your recovery journey. If you are experiencing knee pain, are considering total knee replacement surgery, and would like a consultation, schedule an appointment with Dr. Tauro today!
Knee pain can significantly hinder your daily activities and athletic performance. At Advanced Orthopedics and Sports Medicine Institute (AOSMI), we understand how knee pain can affect your quality of life and are dedicated to restoring your knee strength and mobility and helping you manage your pain. AOSMI’s Dr. Michael Greller has extensive experience effectively treating knee pain and its many causes.
About the Author: Michael J. Greller, MD, MBA, President and Managing Partner of AOSMI, is a Board-Certified Orthopedic Surgeon with Fellowship Training in Sports Medicine, specializing in shoulder, knee, ankle, and hip disorders. Committed to a patient-centered, conservative approach, he helps patients recover swiftly and return to their active lifestyles. He trained at the New York University (NYU) Hospital for Joint Diseases Orthopedic Institute and at Temple University, which afforded him the opportunity to work with high level athletes. Over the course of his career, he has worked with collegiate and professional athletes across disciplines, including dance, football, basketball, and tennis. He has worked as a physician with the U.S. Open Tennis Tournament, Temple Football and Basketball, and the Alvin Ailey Dance Theater. Dr. Greller’s experience with professional athletes uniquely equips him to offer world-class care, meticulously tailored to your specific needs. Dr. Greller excels in advanced minimally invasive techniques and innovative procedures such as the BEAR ACL Implant, the MACI cartilage repair, orthobiologics, and regenerative medicine.
Causes of Knee Pain
Knee pain can stem from various issues, including sports injuries, degenerative conditions, and overuse injuries. In this section, we will discuss each cause of knee pain and its symptoms in detail.

Overuse Injuries:
- Patellofemoral Pain Syndrome: Also known as “runner’s knee,” or jumper’s knee, this condition results from repetitive motion and stress on the knee joint. Patients experience a dull pain felt at the front of the knee, particularly behind or around the kneecap. Athletes often experience this, especially when improper alignment or muscle imbalance exacerbates it.
- Patellar Tendonitis: Also part of “runner’s knee” or “jumper’s knee,” this condition is also common among athletes who frequently run and jump. It involves inflammation of the patellar tendon, which connects the kneecap to the shinbone; the patellar tendon works with the muscles in the front of your thigh to allow you to straighten your knee, allowing you to run, jump, and kick. Symptoms include pain around the kneecap during running and jumping. The main pain in patellar tendonitis is usually sharp and localized to just below the kneecap. It often intensifies during activities that involve jumping, running, or sudden changes in direction. The pain is also felt when the tendon is pressed or palpated, and it can be more pronounced during or after physical activity.
- Iliotibial Band Syndrome (ITBS): When the iliotibial band, a thick band of tissue running from the hip to the shin, becomes tight or inflamed, it causes ITBS. It commonly affects runners and cyclists, causing pain on the outside of the knee.
- Stress Fractures: Stress fractures are tiny cracks in the bone that occur due to repetitive force or overuse, often seen in athletes engaged in high-impact sports such as running or basketball. In the knee, stress fractures can develop in the patella (kneecap) or the tibia (shinbone). Symptoms include localized pain that worsens with activity and improves with rest, swelling, and tenderness. Early diagnosis and management are crucial to prevent the fractures from worsening, which may include rest, modified activity, and physical therapy to address any contributing biomechanical issues.
Sports Injuries:
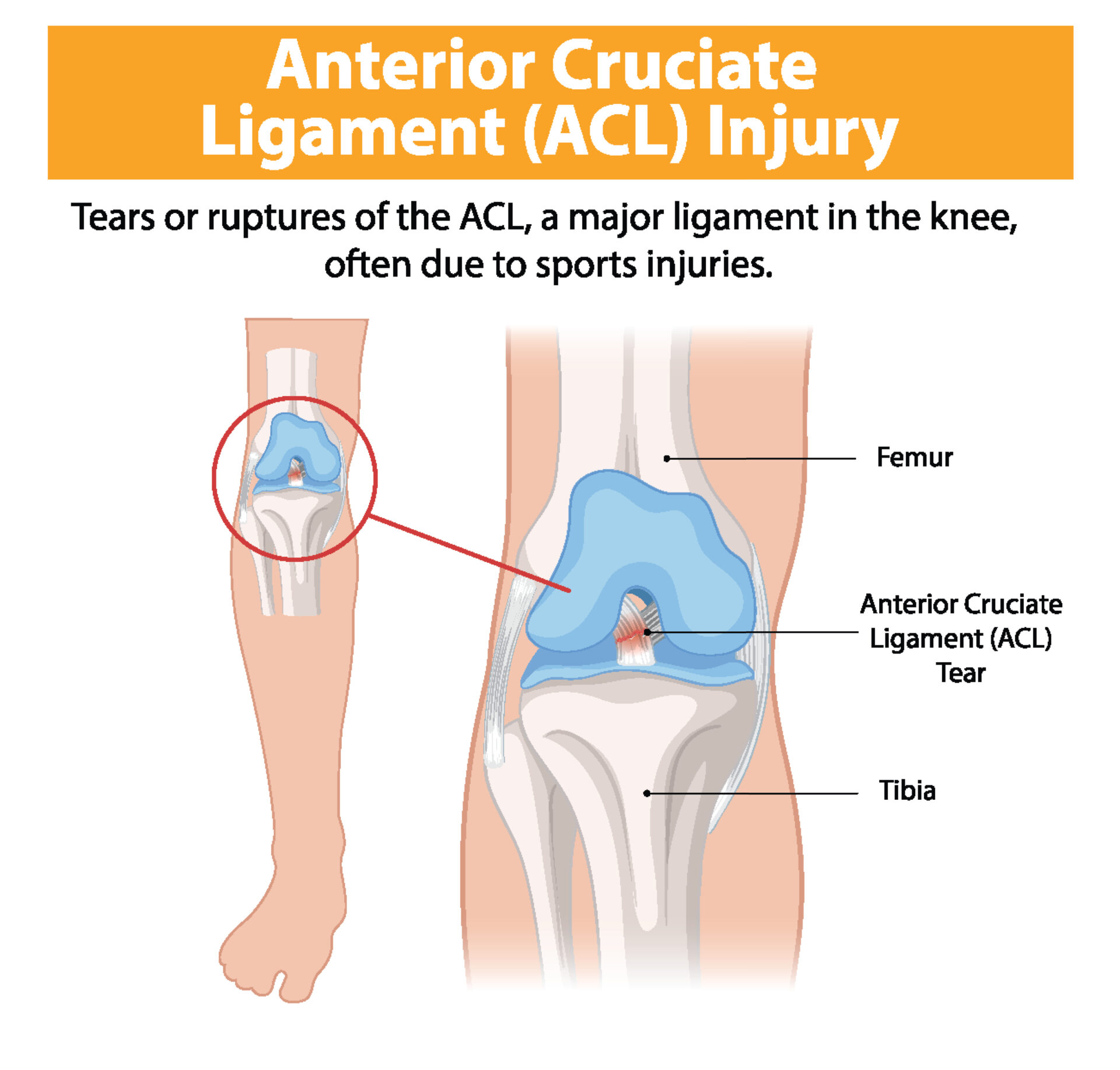
- ACL Tears: The Anterior Cruciate Ligament (ACL) stabilizes the knee during rotational movements. ACL tears often occur in sports that involve sudden stops and changes in direction, like soccer, basketball, skiing, and pickleball. When you tear your ACL, you may hear a loud “pop.” Symptoms include severe pain, rapid swelling, and instability.
- Meniscus Tears: The menisci are C-shaped pieces of cartilage that act as shock absorbers in the knee joint. Twisting or turning quickly, often with the foot planted and the knee bent, can cause tears. Symptoms include pain, swelling, clicking, and difficulty moving the knee
- MCL Injuries: The Medial Collateral Ligament (MCL) runs along the inner part of the knee and helps stabilize it. MCL injuries often result from a direct blow to the outside of the knee, common in contact sports like football and hockey. Symptoms include pain, swelling, and a feeling of instability in the knee.
Degenerative Conditions:
- Knee Osteoarthritis: This wear-and-tear form of arthritis occurs when the cartilage cushioning the ends of bones in the knee joint gradually deteriorates. This leads to pain, stiffness, and decreased mobility, particularly in older adults.
- Rheumatoid Arthritis: An autoimmune disorder, rheumatoid arthritis causes the body’s immune system to attack its tissues, including the joints. This results in painful swelling, joint deformity, and erosion of bones and cartilage.
Diagnosing Knee Pain with Evaluation and Testing
The importance of a thorough evaluation and proper testing to achieve an accurate diagnosis cannot be overstated. Consult the knee pain experts at AOSMI to ensure you receive a proper diagnosis founded on many years of knowledge and experience.

Evaluation: An orthopedic physician must conduct a thorough evaluation to ensure an accurate diagnosis. This includes:
- Medical History: Discussing your symptoms, activity level, and any previous injuries or conditions with your knee pain specialist.
- Physical Examination: Assessing the range of motion, swelling, tenderness, and stability of the knee.
Tests:
- Joint Aspiration: Also known as arthrocentesis, this involves drawing fluid from the knee joint with a needle. The fluid can be analyzed for signs of infection, gout, or other conditions causing knee pain.
- Diagnostic Imaging: X-rays can reveal bone damage or alignment issues.
- Advanced Diagnostic Imaging: MRI scans provide detailed images of soft tissues, including ligaments, tendons, and cartilage. CT scans offer detailed cross-sectional images of bones and joints. Bone scans detect abnormalities such as fractures, infections, or tumors by using a small amount of radioactive material that highlights areas of bone metabolism, revealing issues not visible on standard X-rays.
Knee Pain Treatment Options
Various treatment options, ranging from conservative (non-surgical) management techniques to advanced surgical interventions, help alleviate knee pain and improve functional strength. Consulting with the orthopedic knee pain specialists at AOSMI will help you find the right treatment option for your circumstances.

- Non-Surgical Knee Pain Treatment:
- RICE: Rest, Ice, Compression, and Elevation (RICE) is a first-line treatment approach for acute knee injuries. Rest the knee to avoid weight-bearing, use ice packs for 20 minutes several times a day (wrapped in a cloth to protect the skin), apply a soft bandage for compression, and elevate the knee above heart level to reduce swelling.
- Activity Modification: It is crucial to reduce or modify activities that exacerbate knee pain. This might involve switching to low-impact exercises such as swimming, cycling, or using an elliptical machine. These activities minimize stress on the knee while maintaining fitness. You should also avoid repetitive knee stressors and incorporate rest periods to prevent overuse injuries.
- Medication Management: Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to manage knee pain by reducing inflammation and providing pain relief. Common over-the-counter NSAIDs include ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin.
- Physical Therapy: Tailored exercises and stretches strengthen the muscles around the knee, improve flexibility, and reduce pain.
- Bracing: Knee braces provide support and stability, particularly for those with ligament injuries or instability.
- Corticosteroid Injections: These anti-inflammatory injections offer significant pain relief by reducing inflammation within the knee joint.
- Surgical Interventions for Knee Issues:
- Joint Preservation Surgery: Key procedures include
- Matrix-Associated Autologous Chondrocyte Implantation (MACI), a cutting-edge regenerative procedure in which the patient’s own cartilage cells, harvested arthroscopically, are cultured and then transplanted into the damaged area for effective repair. MACI works by using a small sample of your own cartilage to grow new cells. These cells are then used to create strong repair tissue for your damaged knee cartilage. MACI can help reduce pain, improve knee function, and provide long-lasting results, helping you get back to the activities you love. These methods help preserve the natural knee joint and delay the need for a total knee replacement, especially beneficial for younger patients.
- Osteochondral Allograft Transplant: this procedure uses donor bone and cartilage plugs to repair large areas of damaged cartilage. It is typically used when there are extensive defects that cannot be repaired using the patient’s own tissue.
- Osteochondral Autograft Transfer System (OATS): this involves transferring bone and cartilage from a non-weight-bearing area of the patient’s own joint to a damaged area. OATS is effective for smaller defects and helps restore the joint surface with the patient’s own tissue, promoting a natural repair.
- Implants: implants are crucial for repairing a variety of injuries and conditions – including repairing cartilage that has become loose in the knees. The direct fixation procedure involves using specialized implants or anchors to secure damaged structures such as cartilage or ligaments directly within the knee joint, promoting stability and optimal healing. In orthopedic procedures, sutures play a crucial role. Sutures are medical threads specially designed to stitch or secure tissues together. In knee cartilage repair, sutures are used to anchor and stabilize loose cartilage fragments back into their original position within the joint. This process restores the integrity of the cartilage surface, which is essential for smooth joint movement and reduced pain during activities.
- Microfracture: an arthroscopic technique that stimulates cartilage regeneration by creating tiny fractures in the underlying bone, encouraging new cartilage growth.
- Osteochondritis Dissecans (OCD) Fixation: is a treatment for cartilage injuries in the knee. This method uses special, bioabsorbable tools like the PLLA Chondral Dart and Bio-Compression Screws to repair the damage. The Chondral Dart secures the cartilage in place without touching sensitive joint surfaces, while the Bio-Compression Screw provides strong, secure fixation for larger injuries without the complications that can come with metal screws. These tools are bioabsorbable, which means that they gradually dissolve in the body, eliminating the need for removal surgery and reducing the risk of irritation. This approach helps the cartilage heal properly, allowing you to return to your normal activities.
- IntraOsseous BioPlasty (IOBP): is a treatment for stubborn bone injuries called bone marrow lesions (BMLs). These can happen from conditions like fractures, osteoarthritis, bone bruises, and dead bone tissue (osteonecrosis). If regular treatments don’t help, IOBP might be the solution. This procedure has two main steps, decompression and injection. Decompression: The damaged area in the bone is carefully decompressed to relieve pressure. Injection: A special mix of healing materials is injected into the area. This mix includes platelet-rich plasma (cPRP) from your own bone marrow, combined with a bone matrix substance. This mix helps your bone heal naturally by providing a structure for new bone to grow, growth factors to stimulate repair, and stem cells to generate new bone tissue. The goal is to relieve pain and improve bone health.
- Arthroscopic Procedures: Minimally invasive arthroscopic surgery involves small incisions and the use of a camera to guide the surgeon. This approach minimizes tissue damage and reduces recovery time.
- Surgeons commonly perform procedures such as ACL reconstruction and meniscus repair arthroscopically.
- Patella Stabilization and Re-alignment Procedures: These procedures address issues with kneecap (patella) instability and misalignment. Techniques may include realigning the patella, tightening or releasing surrounding tissues, and stabilizing the knee joint to prevent dislocations and improve knee function.
- Advanced Surgical Procedures: One of the latest innovations in ACL treatment is BEAR (Bridge-Enhanced ACL Restoration), the first procedure approved by the U.S. Food and Drug Administration (FDA) that enables the body to heal its own torn ACL. This technique uses a special implant to stimulate the body’s natural healing process, offering an alternative to traditional ACL reconstruction. Dr. Greller first performed the BEAR Implant procedure in 2022. Restoring the ligament instead of replacing it has several advantages – clinical studies have shown faster recovery of muscle strength and higher patient satisfaction regarding readiness to return to sport compared to traditional ACL reconstruction, which remains the standard of care today.
- Joint Preservation Surgery: Key procedures include
-
-
- This is a rapidly growing field. Our surgeons are constantly using novel techniques to help patients return to sports and quality of life activities. By integrating the latest advancements and innovative procedures, we strive to provide our patients with the best possible outcomes and the quickest path to recovery.
-
Visit AOSMI for Expert Knee Pain Treatment
If you’re suffering from knee pain, don’t let it limit your life. Our team of orthopedic knee specialists is committed to providing personalized care and utilizing the latest medical advancements. We aim to help you strengthen your knees and manage your knee pain so that you can regain your mobility and return to the activities you love. Schedule an appointment with Dr. Greller at AOSMI today and take a meaningful step towards a higher quality of life.
Here at AOSMI, we stay on the cutting edge of orthopedic technology to provide you with the best treatment, helping you live your strongest life. Using Mako robotic surgery, we offer advanced solutions for knee and hip replacements. In 2022, Dr. Michael Greller and Dr. Garret Sobol performed the BEAR (Bridge-Enhanced ACL Restoration) Implant procedure, the first medical advancement that allows your body to heal its own ACL. Today, we’d like to highlight Dr. Eric Buxbaum, Board-Certified Orthopedic Surgeon, Fellowship Trained in Adult Reconstruction, Hip and Knee Arthroplasty – one of our hip and knee orthopedic specialists. He performs total knee replacement, partial knee replacement, and total hip replacement surgeries using Mako SmartRobotics, from Stryker, the industry leader in orthopedic technology.
Dr. Buxbaum explains the benefits of Mako robotic surgery: “We now can better personalize the surgery and predict implant sizing options with more accuracy before we even enter the operating room. During surgery, we have another set of checks and balances for greater precision. This technology enables us to achieve results that are as close to perfect as possible for our patients. We’re better matching each patient’s normal anatomy for a more natural feel.”
In addition to Dr. Buxbaum, our team of orthopedic specialists, including Dr. Michael Greller, Dr. Alan Nasar, and Dr. Garret Sobol, routinely use Mako SmartRobotics for surgical interventions.
Partial Knee Replacement: Targeted Relief
If you have osteoarthritis confined to a single compartment of your knee, partial knee replacement might be the solution. This procedure is ideal when only one part of your knee is damaged, preserving as much of your natural knee structure as possible. This procedure is recommended when pain and limited mobility are restricted to a specific area, and conservative treatments haven’t provided relief.
During the surgery, the surgeon removes only the damaged portion of your knee cartilage and replaces it with an implant, allowing for quicker recovery and more natural knee function.
Total Knee Replacement: Restoring Mobility
Total Knee Replacement surgery is for adults with mid-to-late stage osteoarthritis of the knee, which causes the protective cartilage in the knee joint to wear down over time, resulting in pain, swelling, and stiffness. This procedure is recommended when severe knee pain hampers daily activities, conservative treatments fail, or joint deformities arise due to injury or illness.
During the surgery, the surgeon removes damaged cartilage and bone and place implants strategically to restore knee alignment and function.
Total Hip Replacement: Comprehensive Restoration

You might need a total hip replacement if you suffer from advanced hip osteoarthritis or significant hip joint damage that results in chronic pain and impaired daily activities. Hip osteoarthritis presents distinctive symptoms such as deep pain in the hip, thigh, or groin, that sometimes radiates to the knee and worsens with activities like walking. You might experience stiffness – especially in the morning or after inactivity, reduced range of motion, and a grating sensation when you move your hip. Other signs include muscle weakness, swelling, tenderness, and joint deformities like bone spurs.
During this procedure, the surgeon replaces the damaged bone and cartilage in your hip joint with prosthetic components, restoring hip function and relieving pain.
Mako SmartRobotics: Enhancing Precision
Mako robotic surgery uses advanced technology to assist our surgeons. Your orthopedic surgeon directs Mako’s robotic arm throughout the procedure, positioning the implant in your joint. Mako does not perform surgery, make decisions on its own, or move without the surgeon guiding it. Mako also allows your surgeon to make adjustments to your plan during surgery as needed.
The Process Unveiled 
Pre-Surgery:
- Scan: We’ll conduct a CT scan of your joint, creating a 3D model.
- Plan: Using this model, we meticulously plan your surgery, accounting for your bone structure, disease severity, alignment, and surrounding tissue to determine implant specifics.
During Surgery:
- Your surgeon, using Mako’s robotic arm, removes arthritic bone and cartilage from your joint.
- AccuStop technology helps your surgeon stay within the boundaries defined in your surgical plan, minimizing excess bone and soft tissue loss.
- Real-time data from Mako helps adjust the surgical plan based on your joint’s movement and tension.
Advantages of Mako Robotic Surgery
Compared to patients who received manual knee and hip replacement surgery, patients who received Mako SmartRobotics-assisted knee and hip replacements experienced:
- Less post-operative pain
- Reduced hospital stays and fewer physical therapy rehabilitation sessions
- Better bone preservation and less soft tissue damage
- Improved physical function, improved survivorship, and lower revision rates
Curious if Mako Total Knee, Mako Partial Knee, or Mako Total Hip is right for you? Please reach out to our dedicated orthopedic team. If you are experiencing knee or hip pain, or any of the symptoms explained above, request an appointment today.
As Fall wraps us in its chilly embrace, you can bet basketball courts and ice skating rinks across New Jersey are buzzing with activity. Whether you’re part of a school team, hitting the court for a bit of fun, or gliding across the ice with friends and family, these Fall sports are a great way to stay active. With all the excitement, there’s also a chance of bumps, bruises, and sometimes more serious injuries. At AOSMI, we believe in patient education. We want to teach you about the more common Fall sports injuries, so that you are prepared and so that we can work together to get you back to your strongest self.
Common Fall Basketball Injuries:
Common Injuries: Some of the most common injuries in basketball are ankle sprains and anterior cruciate ligament (ACL) tears, both of which impact performance and long-term joint health.
Causes of Injury: Ankle sprains arise from the high-impact nature of basketball, particularly during rapid direction changes or awkward landings after jumps. ACL tears are often linked to abrupt stops, pivots, or sudden directional changes, exerting stress beyond the knee joint’s normal capacity.

Treatment and Surgery: Initial treatment for ankle sprains involves the R.I.C.E. protocol (Rest, Ice, Compression, and Elevation) to reduce swelling. ACL tears may necessitate surgical reconstruction using the patient’s tissues or grafts. At AOSMI, we are on the cutting-edge of orthopedic treatment – as such, we offer the BEAR (Bridge-Enhanced ACL Restoration) Implant that allows for natural healing without the need for grafts.
Physical Therapy Rehabilitation: Post-surgery, physical therapy becomes pivotal in restoring strength, flexibility, and joint stability. Progressive exercises targeting muscle strength, balance, and proprioception form the core of rehabilitation, guided by physical therapists to ensure a gradual return to play, minimizing the risk of re-injury. At AOSMI, our physical therapists tailor their treatment plans to your unique injury, ensuring a personalized approach.
Common Fall Ice Skating Injuries:
Common Injuries: Ice skaters frequently contend with fractures, particularly in vulnerable areas like the wrist and hip, because of the dynamic and sometimes acrobatic nature of the sport.
Causes of Injury: Falls on the ice, whether during jumps, spins, or routine skating, expose skaters to the risk of fractures. The hard frozen surface amplifies the impact, leading to fractures, especially in areas like the wrist and hip.

Treatment and Surgery: Immediate immobilization is important for managing fractures sustained during ice skating. Wrist fractures may require casting or splinting, while hip fractures may necessitate surgical intervention, involving plates, screws, or other fixation devices for proper alignment and stability.
Physical Therapy Rehabilitation: Rehab for ice skating injuries takes a comprehensive approach. Range-of-motion exercises are crucial for regaining flexibility, while progressive weight-bearing activities aid in rebuilding strength. Physical therapists craft tailored plans, integrating exercises that address the unique challenges of ice skating injuries, with a focus on enhancing balance, coordination, and functional movement. This personalized rehabilitation aims not only to restore functionality but also to prevent future injuries, facilitating a safe return to the ice.
By addressing the specific Fall sports injuries associated with basketball and ice skating, we aim to equip you with the knowledge needed to navigate the season safely. At AOSMI, our team is committed to providing the highest quality orthopedic and physical therapy care to our patients across New Jersey. If you are experiencing pain or injury from these sports, please request an appointment today. We are dedicated to helping you live a healthier, stronger life.
 Anterior Cruciate Ligament (ACL) injuries are one of the most common knee injuries in the United States – approximately 400,000 ACL injuries occur every year. Historically, orthopedic surgeons have had limited options in treating a torn ACL. In ACL reconstruction, today’s standard of care, the surgeon completely removes the remaining torn ACL and reconstructs it with either a tendon from the patient’s own leg (called an autograft) or a deceased donor (called an allograft).
Anterior Cruciate Ligament (ACL) injuries are one of the most common knee injuries in the United States – approximately 400,000 ACL injuries occur every year. Historically, orthopedic surgeons have had limited options in treating a torn ACL. In ACL reconstruction, today’s standard of care, the surgeon completely removes the remaining torn ACL and reconstructs it with either a tendon from the patient’s own leg (called an autograft) or a deceased donor (called an allograft).
At Advanced Orthopedic Sports Medicine Institute (AOSMI), we are now offering a new technology called the BEAR® (Bridge-Enhanced ACL Restoration) Implant. The BEAR Implant is the first medical advancement granted approval from the U.S. Food and Drug Administration (FDA) that enables the body to heal its own torn ACL. This new approach is a paradigm shift from ACL reconstruction and is the first innovation in ACL tear treatment in more than 30 years.
AOSMI completed the first official procedure on November 15, 2022. Michael J. Greller, MD, MBA, CPE, FAAOS, a Board-Certified Orthopedic Surgeon who is Fellowship-trained in Sports Medicine led the procedure. He was assisted by Garret L. Sobol, MD, Board-Certified Orthopedic Surgeon who is also Fellowship-trained in Sports Medicine.
“There are a number of advantages to restoring a ligament instead of replacing it, and the BEAR Implant is an exciting medical technology that is the first to clinically demonstrate that it enables healing of the patient’s torn ACL while maintaining the natural knee anatomy,” said Dr. Greller “Encouraging clinical studies have shown faster recovery of muscle strength and higher patient satisfaction with regard to readiness to return to sport than traditional ACL reconstruction – the standard of care today.”
ACL Injuries – An Overview
Your knee joint is formed by three bones: the femur (thigh bone), tibia (shin bone), and patella (kneecap). The ACL (Anterior Cruciate Ligament) is one of the four main ligaments in the knee that helps to stabilize the joint. It is located in the center of the knee – it runs from the backside of the femur (thigh bone) to the front of the tibia (shin bone). The ACL is responsible for preventing the tibia from sliding out in front of the femur, and helping to control rotational movements of the knee.
The majority of ACL injuries are non-contact injuries – when athletes while running, rapidly change directions, stop or decelerate, or land from a jump without properly bending their knees. ACL injuries can also occur from direct contact to the knee joint. Most ACL injuries are complete tears, in which the ligament has been torn in half or pulled directly off the bone.
Patients usually report hearing and feeling a popping sensation during the injury. After the tear, patients experience pain with swelling, instability of the joint, loss of full range of motion, tenderness, and discomfort while walking.
ACL injury treatment is focused on preventing further knee instability and protecting the joint from further trauma. The two approaches to treatment are the non-surgical approach and the surgical approach. The approach is dependent on the extent of damage to the knee and the patient’s willingness to modify activity. Young and competitive athletes who want to return to activities that require aggressive jumping, cutting and pivoting or deceleration movements, and patients with meniscal tears usually pursue surgical reconstruction. Patients who have partial tears, do not have knee instability, and don’t partake in these “at-risk” movements can maintain their knee stability with physical therapy and rehabilitation alone. However, physical therapy is a core component of ACL treatment, surgical or non-surgical. For complete tears, surgery is usually recommended.
Standard ACL Reconstruction vs. BEAR Implant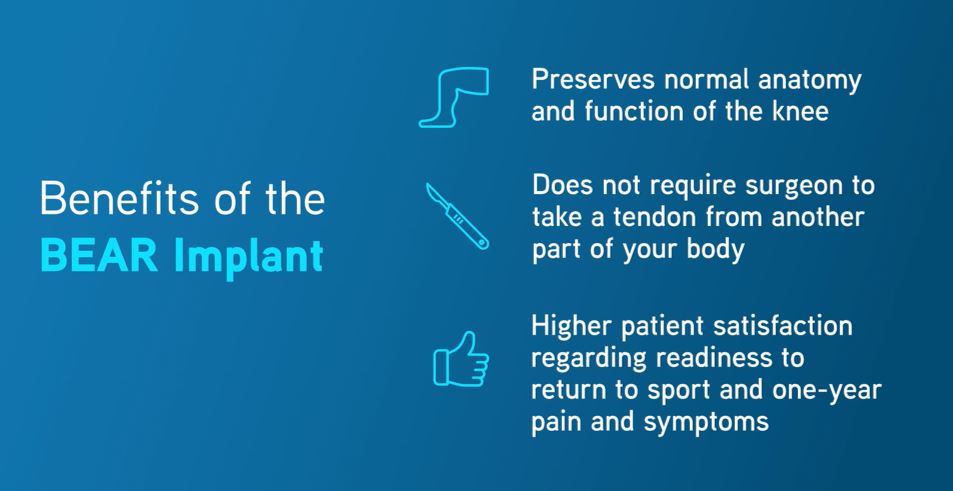
ACL reconstruction surgery remains the gold standard of care. In this procedure, the surgeon takes tendon from the patient’s patellar tendon (patellar tendon autograft), hamstring tendon (hamstring tendon autograft), or from a human donor (allograft) to replace the torn ACL.
Unlike reconstruction, the BEAR Implant does not require a second surgical wound site to remove a healthy tendon from another part of the leg or the use of a donor tendon. The BEAR Implant acts as a bridge to help ends of the torn ACL heal together. The surgeon injects a small amount of the patient’s own blood into the implant and inserts it between the torn ends of the ACL in a minimally invasive procedure. The combination of the BEAR Implant and the patient’s blood enables the body to heal the torn ends of the ACL back together while maintaining the ACL’s original attachments to the femur and tibia. As the ACL heals, the BEAR Implant is reabsorbed by the body, within approximately eight weeks.
BEAR Implant – Clinical Evidence
Safety and effectiveness of the BEAR Implant is supported by clinical evidence. As shown in Murray et. al 2019, IKDC scores, a patient-completed tool which contains sections on knee symptoms, function, and sports activities, from the BEAR Implant procedure was similar to that of ACL reconstruction two years post-surgery. AP Laxity, which measures stability of the knee joint, is the same as ACL reconstruction two years post-surgery. The BEAR Implant provides statistically better hamstring strength at 6 and 12 months, with the trend sustained to 2 years. BEAR Implant patients were also more likely to experience fewer contralateral ACL tears (tears in the non-injured knee) at two years. MRI indicates that the BEAR implant facilitates healing of the native ACL so that its size, geometry, and tissue composition are more like native ACL tissue than autograft. 86 percent of BEAR patients returned to pivoting sports by one year.
Risks and Limitations of the BEAR Implant
Following the BEAR Implant, patients are directed to follow the BEAR Implant physical therapy program. The BEAR Implant has the same potential medical and surgical complications as other orthopedic surgical procedures, including ACL reconstruction. These include the risk of re-tear, infection, knee pain, meniscus injury and limited range of motion. The BEAR Implant is indicated for skeletally mature patients at least 14 years of age with a complete rupture of the ACL, as confirmed by MRI. Patients must have an ACL stump attached to the tibia to construct the repair. The BEAR device must be implanted within 50 days of injury.
If you meet these criteria, you may be a candidate for the BEAR Implant procedure. To learn more about the procedure, request an appointment. If you have questions about ACL tears or if you are experiencing knee pain, contact us. With offices across New Jersey, the physicians and staff of Advanced Orthopedic Sports Medicine Institute are committed to restoring your health so that you can get back to your active lifestyle as quickly and safely as possible. To learn more about how you can benefit from expert orthopedic treatment, call us (732.720.2555) or request an appointment today.


Christian Contreras developed a strong passion for soccer at just four year’s old. His father was a semi-pro soccer player, so his love for the game was something that was in his blood. He often dreamed of becoming a professional soccer player.
By age twelve, Christian gained recognition from top-tier programs in the state. At fourteen, he was scouted to play for Philadelphia Union Academy. During his three years with the academy, he was called up to national team combines allowing him to play at the highest levels for his age.
In March 2016, Christian tore his left ACL (Anterior Cruciate Ligament) that was further complicated by pulled hamstrings. These injuries set him back nearly 13 months before he could return to playing. The timing of these injuries couldn’t be worse seeing that these were critical months for college scouting.
Despite the setbacks, Christian returned to playing competitively his senior year and with great excitement, he committed to Temple University, where he had hopes of making a name for himself quickly.
Spring and summer training prior to his first semester at Temple was rigorous. On June 5th, during an early Summer League game, Christian was dribbling in the midfield when two players tackled him for the ball. He jumped up to avoid their kicks and when he landed awkwardly on his right leg. He quickly got up and walked himself off the field. While in great pain, he was really hoping it wasn’t anything serious. He thought it was only a minor injury.
Christian sought the guidance of Sports Medicine Specialist, Dr. Gerardo Goldberger, from AOSMI in Freehold, NJ. Dr. Goldberger brought in his colleague, Dr. Michael Greller, also a Sports Medicine specialist, who delivered the news that he had in fact torn his ACL once again.
Christian was devasted, but it didn’t take long for his despair to turn into optimism. Dr. Greller educated Christian on what caused his injury and how he was going to repair the ACL. The doctor gave him confidence that his procedure and recovery would go well and that he was likely to recover fully.
Post surgery, after five months of rehabilitation, Dr. Greller is very impressed with the way Christian is healing and he is expected to recover fully. His goal is to be cleared to play sometime early in the spring with the main focus of being at peak performance for the Fall season next semester.
Christian Contreras doing drills less than 4 weeks after ACL surgery.
“Dr. Greller instills confidence in me every time I see him and I believe that by following his recovery plan, I will be as good as new by Spring,” notes Christian.
Childhood dreams of becoming a professional soccer player haven’t been derailed by injury. In fact, dreams may be closer to reality for Christian thanks to proper medical care and his lifelong passion for the game!
By Jeffrey White









