Total hip replacement has come a long way, with modern techniques providing faster recovery and less post-operative pain. Two groundbreaking approaches, the Direct Anterior Approach and the Mini Posterior Approach, are leading the future of hip replacement surgery, offering patients greater comfort and quicker healing times. Let’s explore these options.
Direct Anterior Approach Total Hip Replacement Surgery
The Direct Anterior Approach is a minimally invasive technique that avoids cutting through major muscles, reducing trauma to the body. This approach allows patients to recover faster and experience less pain after surgery. By preserving more of the surrounding tissues, the Direct Anterior Approach also promotes early mobility and a lower risk of dislocation.
What is the recovery time for Direct Anterior Approach hip replacement?
Patients can often return to regular activities within 4-6 weeks, with minimal restrictions.
Mini Posterior Approach
The Mini Posterior Approach is another innovative technique that provides excellent access to the hip joint with a smaller incision. This method involves less cutting of muscle and tendons compared to traditional surgeries, resulting in quicker recovery times and less postoperative discomfort. It is known for being less complex, making it a popular choice for many patients.
Is the Mini Posterior Approach safe for all patients?
Yes, but it’s essential to consult with your surgeon to determine if it’s the best option for your condition.
Benefits of These Approaches
Innovations in surgery have provided a wide array of benefits for patients. Some of these advantages include:
- Faster recovery and return to normal activities
- Less post-operative pain
- Smaller incisions with minimal scarring
- Reduced risk of complications such as dislocation
Contact an Expert Surgeon Today
If you’re considering hip replacement surgery, trust Advanced Orthopedic and Sports Medicine Institute (AOSMI) for cutting-edge treatments and expert care. We serve patients throughout New Jersey. We have convenient locations in Freehold, Monroe Township, Toms River, Belmar, Edison, and Manalapan, NJ. Reach out today to learn more about your options.
We are thrilled to announce that several esteemed physicians from Advanced Orthopedics and Sports Medicine Institute (AOSMI) have been recognized as NJ Top Docs for 2024. This prestigious honor underscores our commitment to providing exceptional orthopedic care and advanced treatment options for our patients in New Jersey.
About the Top Docs Awards
The Top Docs awards are based on a rigorous selection process. Nominees complete a comprehensive qualification questionnaire covering their education, training, years in practice, continuing education, licensing, publications, charitable work, professional appointments, and achievements. Each component is verified to ensure that nominees meet the high standards set by the Top Docs organization. Board certification is required for applicable specialties, and nominees must also undergo a thorough review of malpractice and licensing records to confirm there are no serious issues. Patient reviews are collected and compiled to provide a comprehensive assessment of each nominee’s performance.
Join us in celebrating the remarkable accomplishments of the following Top Docs nominees:

Michael J. Greller, MD, MBA, CPE, FAAOS
Dr. Michael J. Greller is a Board-certified orthopedic surgeon specializing in sports medicine and joint preservation. His comprehensive approach to patient care, combined with his administrative expertise, has established him as a leader in orthopedic surgery. Dr. Greller’s commitment to excellence is evident in both his clinical and organizational contributions to AOSMI.

Ali Valimahomed, MD, FAAPMR
Dr. Ali Valimahomed is a dual Board-certified specialist in Pain Medicine and Physical Medicine & Rehabilitation. His expertise lies in comprehensive pain management and restoring function to patients suffering from chronic pain conditions. Dr. Valimahomed’s holistic approach and dedication to improving patients’ quality of life make him a standout in his field.

Alison Dewaters, DPM, FACFAS
Dr. Alison Dewaters is a Board-certified podiatric surgeon with a focus on reconstructive foot and ankle surgery. As a Fellow of the American College of Foot and Ankle Surgeons, Dr. Dewaters is renowned for her surgical precision and compassionate patient care, ensuring optimal outcomes for her patients.

Arth Patel, MD, MPH
Dr. Arth Patel is a Board-certified Primary Care Sports Medicine physician with a background in Family Medicine. He is dedicated to the non-operative management of musculoskeletal injuries, promoting wellness and injury prevention. Dr. Patel’s patient-centered approach and emphasis on holistic care have earned him a well-deserved place among NJ’s top doctors.

Eric Buxbaum, DO, FAAOS
Dr. Eric Buxbaum is a Board-certified orthopedic surgeon with expertise in hip and knee replacement surgery. His focus on advanced surgical techniques and patient-centric care has made him a trusted name in joint health. Dr. Buxbaum’s approach combines precision with compassion, ensuring his patients receive the best possible care.

Joseph Tauro, MD
Dr. Joseph Tauro is a nationally recognized expert in shoulder, sports and degenerative joint disorders, known for his pioneering techniques in arthroscopic surgery. As a Board-certified Orthopedic Surgeon, Dr. Tauro’s contributions to the field have set new standards in patient care and surgical excellence. His innovative approach ensures that patients receive the most advanced and effective treatments available.

Stacey Gallacher, MD, FAAOS
Dr. Stacey Gallacher is a dual Board-certified orthopedic surgeon specializing in shoulder and elbow surgery and trauma care. Her precise surgical skills and compassionate patient care have made her a trusted specialist in her field. Dr. Gallacher’s dedication to improving patient outcomes through both surgical and non-surgical interventions is commendable.

Gerardo Goldberger, DO, FAOAO
Dr. Gerardo Goldberger is a Board-Certified orthopedic surgeon and Fellow of the American Osteopathic Academy of Orthopedics. His specialization in sports medicine and arthroscopic surgery allows him to effectively treat a wide range of athletic injuries. Dr. Goldberger’s dedication to his patients and innovative treatment methods make him a top choice for orthopedic care.

David Kirschenbaum, MD
Dr. David Kirschenbaum is an hand and upper extremity Fellowship-Trained orthopedic surgeon. His extensive experience and commitment to cutting-edge techniques provide patients with innovative solutions for their orthopedic needs. Dr. Kirschenbaum’s dedication to excellence is reflected in his high patient satisfaction and successful surgical outcomes.

At AOSMI, we are incredibly proud of our doctors’ achievements and their unwavering commitment to providing the highest quality of orthopedic care. Being named NJ Top Docs is a testament to their expertise, compassion, and dedication to patient well-being. We extend our heartfelt congratulations to each of these outstanding physicians and look forward to their continued success in advancing orthopedic and sports medicine.
For more information or to schedule an appointment with any of our top doctors, please contact our office at (732) 335-6727 and schedule an appointment online. Together, we can achieve better health and a higher quality of life.
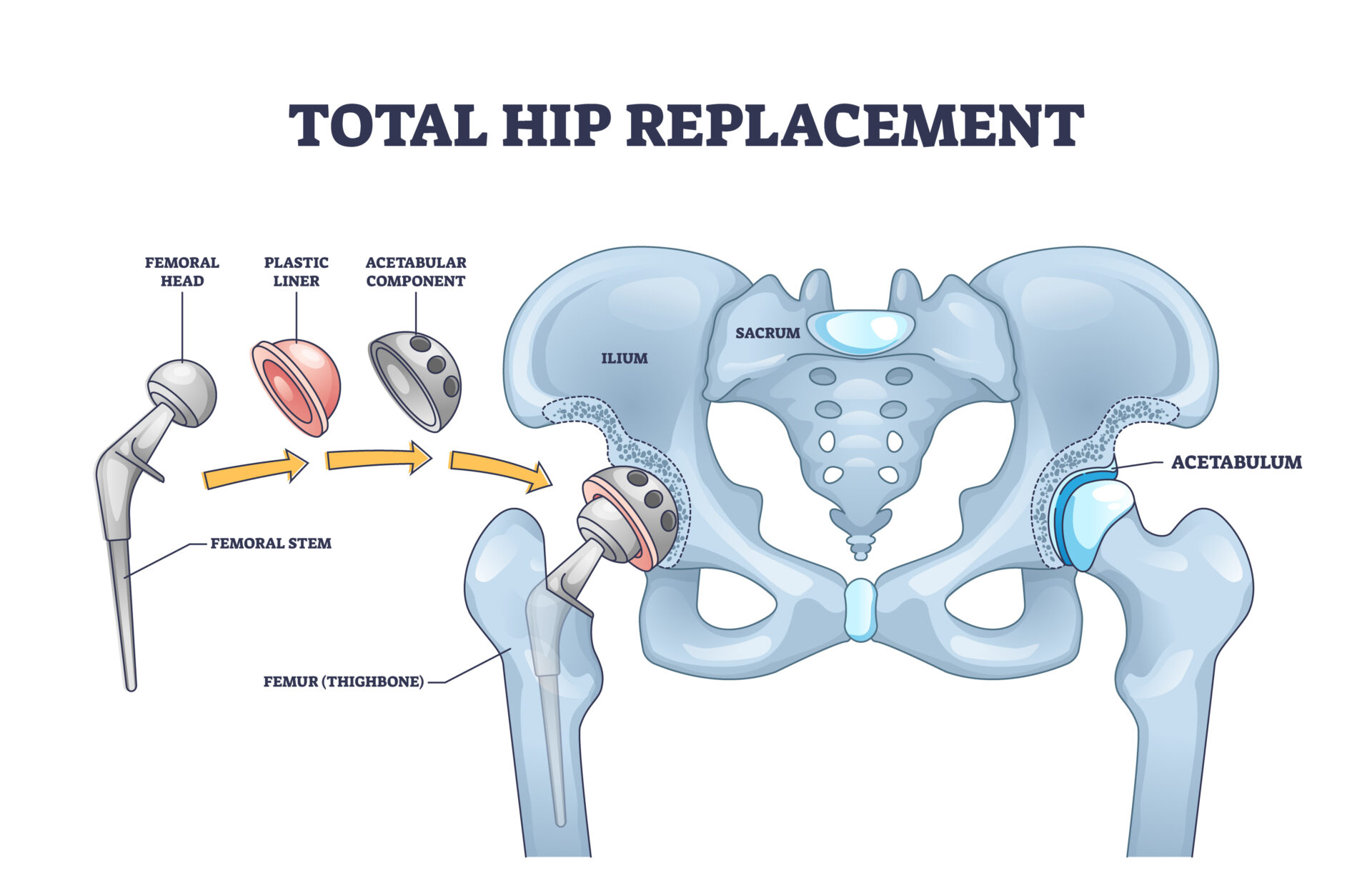
Total hip replacement is a common surgical procedure for individuals suffering from severe hip arthritis or injury. This surgery involves replacing the damaged hip joint with an artificial implant to relieve pain and restore function. This comprehensive guide will help you understand total hip replacement surgery, including pre-surgery preparation, what to expect on the day of surgery, and post-surgery recovery.
About the Author: Joseph Tauro, MD, a Board-Certified orthopedic surgeon, is nationally recognized for his expertise in treating shoulder, sports, and degenerative joint disorders. As a professor at Rutgers Medical School and a Master Instructor for the Arthroscopy Association of North America (AANA), he leads the field in developing new techniques for minimally invasive joint replacement, arthroscopic shoulder surgery, and Augmented Reality surgical training. Patients from across the U.S. are referred to Dr. Tauro for his specialized care. Request an appointment with Dr. Tauro today to experience expert orthopedic care first-hand!
Anterior Approach Total Hip Replacement
Dr. Tauro almost always utilizes an Anterior Approach for hip replacement surgery. No muscles are cut using this technique and the chance of a postoperative dislocation is greatly reduced. You will not need any braces or pillows between the legs with an anterior hip replacement.
Pre-Surgery Guidelines for Total Hip Replacement
What You Should Do Before Hip Replacement Surgery:
Consultation with Dr. Tauro:
- Have a thorough discussion with your surgeon about the procedure, risks, and benefits of total hip replacement surgery.
Medical Clearance and Preparation:
- Obtain medical clearance from your primary care physician if required.
- Review all medications with your doctor. You may need to stop certain medications, like blood thinners, a few days before surgery.
Physical and Home Preparation:
- Engage in pre-surgery physical therapy or a home therapy program if recommended to strengthen the hip muscles before hip replacement surgery.
- Arrange your home to accommodate your post-surgery needs. This might include setting up a comfortable resting area and ensuring easy access to necessities. You may need a walker or crutches for assistance after surgery.
What You Shouldn’t Do Before Hip Replacement Surgery:
Eating and Drinking:
- Do not eat or drink anything after midnight before your hip surgery day. This includes chewing gum, which can produce excessive saliva in your stomach.
Smoking and Alcohol:
- Avoid smoking as it can impair healing and increase the risk of complications.
- Do not consume alcohol at least 24 hours before hip replacement surgery.

Day of Total Hip Replacement Surgery
What to Do on the Day of Surgery:
Arrive on Time:
- Arrive at the hospital or surgical center at the scheduled time. The surgery center will call you with that time generally the day before your hip replacement surgery.
Wear Comfortable Clothing:
- Wear loose, comfortable clothing that is easy to remove and put on.
Bring Essentials:
- Bring necessary documents and a list of medications.
What to Expect on the Day of Surgery:
Pre-Operative Preparation:
- You will undergo pre-operative preparations, including vital sign checks and anesthesia administration. Anesthesia will usually include a mixture of specialized local anesthetics placed in the surgical site to numb the hip as well as spinal anesthesia.
Surgery Duration:
- The procedure typically takes 1-2 hours, but this can vary depending on the complexity of the hip replacement surgery.
Post-Operative Recovery:
- After surgery, you will be monitored in a recovery area until the anesthesia wears off.
Post-Operative Care and Recovery After Total Hip Replacement
Immediate Post-Op Care:
- Almost all hip replacements are considered outpatient procedures. You may go home the same day or we may keep you overnight if your operation was done in the hospital. Regardless, we will have you out of bed and in a chair the day of surgery and walking with a walker or crutches the same day or the morning after the surgery.
- We DO NOT send patients to inpatient rehabilitation facilities as we feel infection rates are higher and care is inconsistent. You are much better off at home in a clean, comfortable and familiar environment.
- You will need to make sure a friend or family member is with you for the first 2 days after discharge.
- We will make arrangements for physical therapy in your home for the first week or 2 after surgery. You will be given a prescription for outpatient therapy after your first visits with us 1 week after your surgery.
Prevention of Blood Clots:
- Please take an 81mg “baby” aspirin twice a day for three weeks after your surgery.
- If you are on stronger blood thinners (such as Elaquis or Xarelto) you should restart them the day after surgery.
Pain Management:
- Expect some pain and discomfort, which will be managed with prescribed medications. With the regional block, there is usually minimal pain initially, which can be managed with Tylenol and ibuprofen afterward. When the local anesthetics we use after the surgery wears off a few days after surgery, pain may increase and you may need stronger pain medication which we will prescribe. Make sure the hospital or surgery center has accurate information about your pharmacy.
Brace and Crutch Usage:
- You will likely need crutches or a walker to assist with walking after knee replacement surgery. Weight bearing is usually permitted immediately and progression to a cane and ultimately no assist will take place as soon as your comfort and stability is achieved
Follow-Up Appointments:
- Schedule follow-up appointments with your surgeon, usually 1 week post-surgery. You can pre-schedule this appointment in our office before your hip replacement surgery.

Phases of Recovery After Total Hip Replacement Surgery:
Phase 1 (0-2 Weeks): Protection and Initial Healing
- Use crutches or a walker as directed.
- Engage in your home therapy exercises as prescribed by Dr. Tauro and your physical therapist.
- Full weight bearing is usually permitted. Ice on the hip incision can be helpful to reduce swelling.
Phase 2 (2-6 Weeks): Normalizing your gait
- Gradually increase mobility exercises under the guidance of your physical therapist.
- Isometric exercises and some light strengthening will be started by your physical therapist
- Focus on progressing to a cane or no assist if deemed safe by your therapist.
Phase 3 (6-12 Weeks): Strengthening
- Incorporate progressive strengthening exercises for the hip and surrounding muscles.
- Continue to avoid heavy lifting or activities that place excessive strain on the hip.
Phase 4 (3-6 Months): Functional Training
- Progress to functional and everyday activities as tolerated.
- Aim to return to normal activities gradually, following your therapist’s advice.
Full Recovery After Total Hip Replacement Surgery:
Time Frame:
- Full recovery can take anywhere from 4-6 months to a year, depending on the extent of the surgery and your adherence to the rehabilitation program. Most patients can return to activities like walking and light exercise at 6-12 weeks post-op
Rehabilitation:
- Consistent and dedicated rehabilitation is crucial for a successful outcome. Attend all therapy sessions and follow your doctor’s and therapist’s instructions diligently.

Frequently Asked Questions (FAQs):
How long will I need to use crutches or a walker after hip replacement surgery?
- Typically, you will need to use crutches or a walker for 2-4 weeks to support your hip.
When can I return to work after total hip replacement surgery?
- This depends on your job and the extent of your surgery. Desk jobs may allow a return within a few weeks, while more physical jobs may require several months.
Will I regain full range of motion and function after hip replacement surgery?
- With proper rehabilitation, most patients regain an excellent range of motion and hip function, though individual results can vary.
Total hip replacement surgery is a highly effective procedure for treating severe hip arthritis and injury. By following the pre-surgery guidelines, preparing adequately, and adhering to the post-operative care and rehabilitation phases, you can achieve a successful recovery and regain full function of your hip. Always communicate with Dr. Tauro and our team of orthopedic experts at AOSMI if you have any concerns during your recovery journey. If you are experiencing hip pain, are considering total hip replacement surgery, and would like a consultation, schedule an appointment with Dr. Tauro today!
Here at AOSMI, we stay on the cutting edge of orthopedic technology to provide you with the best treatment, helping you live your strongest life. Using Mako robotic surgery, we offer advanced solutions for knee and hip replacements. In 2022, Dr. Michael Greller and Dr. Garret Sobol performed the BEAR (Bridge-Enhanced ACL Restoration) Implant procedure, the first medical advancement that allows your body to heal its own ACL. Today, we’d like to highlight Dr. Eric Buxbaum, Board-Certified Orthopedic Surgeon, Fellowship Trained in Adult Reconstruction, Hip and Knee Arthroplasty – one of our hip and knee orthopedic specialists. He performs total knee replacement, partial knee replacement, and total hip replacement surgeries using Mako SmartRobotics, from Stryker, the industry leader in orthopedic technology.
Dr. Buxbaum explains the benefits of Mako robotic surgery: “We now can better personalize the surgery and predict implant sizing options with more accuracy before we even enter the operating room. During surgery, we have another set of checks and balances for greater precision. This technology enables us to achieve results that are as close to perfect as possible for our patients. We’re better matching each patient’s normal anatomy for a more natural feel.”
In addition to Dr. Eric Buxbaum, our team of orthopedic specialists, including Dr. Michael Greller, Dr. Alan Nasar, and Dr. Garret Sobol, routinely use Mako SmartRobotics for surgical interventions.
Partial Knee Replacement: Targeted Relief
If you have osteoarthritis confined to a single compartment of your knee, partial knee replacement might be the solution. This procedure is ideal when only one part of your knee is damaged, preserving as much of your natural knee structure as possible. This procedure is recommended when pain and limited mobility are restricted to a specific area, and conservative treatments haven’t provided relief.
During the surgery, the surgeon removes only the damaged portion of your knee cartilage and replaces it with an implant, allowing for quicker recovery and more natural knee function.
Total Knee Replacement: Restoring Mobility
Total Knee Replacement surgery is for adults with mid-to-late stage osteoarthritis of the knee, which causes the protective cartilage in the knee joint to wear down over time, resulting in pain, swelling, and stiffness. This procedure is recommended when severe knee pain hampers daily activities, conservative treatments fail, or joint deformities arise due to injury or illness.
During the surgery, the surgeon removes damaged cartilage and bone and place implants strategically to restore knee alignment and function.
Total Hip Replacement: Comprehensive Restoration

You might need a total hip replacement if you suffer from advanced hip osteoarthritis or significant hip joint damage that results in chronic pain and impaired daily activities. Hip osteoarthritis presents distinctive symptoms such as deep pain in the hip, thigh, or groin, that sometimes radiates to the knee and worsens with activities like walking. You might experience stiffness – especially in the morning or after inactivity, reduced range of motion, and a grating sensation when you move your hip. Other signs include muscle weakness, swelling, tenderness, and joint deformities like bone spurs.
During this procedure, the surgeon replaces the damaged bone and cartilage in your hip joint with prosthetic components, restoring hip function and relieving pain.
Mako SmartRobotics: Enhancing Precision
Mako robotic surgery uses advanced technology to assist our surgeons. Your orthopedic surgeon directs Mako’s robotic arm throughout the procedure, positioning the implant in your joint. Mako does not perform surgery, make decisions on its own, or move without the surgeon guiding it. Mako also allows your surgeon to make adjustments to your plan during surgery as needed.
The Process Unveiled 
Pre-Surgery:
- Scan: We’ll conduct a CT scan of your joint, creating a 3D model.
- Plan: Using this model, we meticulously plan your surgery, accounting for your bone structure, disease severity, alignment, and surrounding tissue to determine implant specifics.
During Surgery:
- Your surgeon, using Mako’s robotic arm, removes arthritic bone and cartilage from your joint.
- AccuStop technology helps your surgeon stay within the boundaries defined in your surgical plan, minimizing excess bone and soft tissue loss.
- Real-time data from Mako helps adjust the surgical plan based on your joint’s movement and tension.
Advantages of Mako Robotic Surgery
Compared to patients who received manual knee and hip replacement surgery, patients who received Mako SmartRobotics-assisted knee and hip replacements experienced:
- Less post-operative pain
- Reduced hospital stays and fewer physical therapy rehabilitation sessions
- Better bone preservation and less soft tissue damage
- Improved physical function, improved survivorship, and lower revision rates
Curious if Mako Total Knee, Mako Partial Knee, or Mako Total Hip is right for you? Please reach out to our dedicated orthopedic team. If you are experiencing knee or hip pain, or any of the symptoms explained above, request an appointment today.
Authored by Dr. Arth Patel, MD, our expert board-certified Sports Medicine physician. Dr. Patel is known for his dedication to providing compassionate and exceptional care. With specialized knowledge in treating sports-related injuries and managing both acute and chronic conditions, Dr. Patel is committed to helping people of all ages achieve optimal musculoskeletal health.
What Is Piriformis Syndrome?
Piriformis syndrome happens when a muscle deep in your buttock, called the piriformis, gets tight or spasms, causing pain. This is commonly confused sciatica. The piriformis muscle is under the glute muscles and is important for moving your hips and keeping your balance. It helps turn your hip outward and lift your leg to the side. If this muscle becomes fatigued or biomechanics change, it can cause issues with how you stand or walk and lead to other problems.
Research shows that up to 17% of people with chronic low back pain might have piriformis syndrome. Understanding the symptoms, causes, and treatment options for piriformis syndrome is crucial for athletes experiencing these symptoms seeking effective orthopedic care. In this article, we will explore the ins and outs of piriformis syndrome and discuss various treatment approaches to help alleviate pain and improve quality of life.

Recognizing the Symptoms of Piriformis Syndrome
Recognizing the symptoms of piriformis syndrome is the first step in understanding and addressing this condition. The most common symptom is pain, which may be localized in the buttocks. It is sometimes confused with sciatica, which causes a sharp shooting pain down the back of the leg. Although both can happen together, it is very rare. This pain is often described as a deep ache or sharp shooting sensation.
Other symptoms that may accompany piriformis syndrome include difficulty sitting (wallet sign) or walking for extended periods. Some individuals may also experience muscle weakness or difficulty in moving their leg or foot. This pain usually affects one side more and can get worse with sitting too long, moving your hip often, like when walking or climbing stairs, or if you press on the sore area.
It’s important to note that the symptoms of piriformis syndrome can be similar to those of other conditions, such as sciatica or lumbar radiculopathy. Seeking an accurate diagnosis from a board-certified primary care sports medicine physician, orthopedic surgeon or physiatrist is crucial to obtain an accurate diagnosis before starting any treatment.
Causes of Piriformis Syndrome
Understanding the causes and risk factors of piriformis syndrome can help active individuals and athletes prevent or manage this condition more effectively. While the exact cause of piriformis syndrome is often unknown, there are several factors that may contribute to its development.
One possible cause of piriformis syndrome is excessive tightness or spasm of the piriformis muscle itself. This can be triggered by overuse, improper exercise technique, or trauma to the buttocks region.
In some cases, anatomical variations or abnormalities may also play a role. For example, having a sciatic nerve that runs through the piriformis muscle or having a variation in the shape or position of the piriformis muscle itself can increase the risk of developing piriformis syndrome.
Other factors that may increase the risk of piriformis syndrome include muscle imbalances, poor posture, and prolonged sitting or engaging in repetitive activities that involve the piriformis muscle.

Piriformis Syndrome Treatment Options
Once one of our doctors has confirmed a diagnosis of piriformis syndrome, there are several treatment options available to alleviate symptoms, reduce pain, and promote recovery. The choice of treatment will depend on the severity of your condition and your individual needs.
- Conservative treatments: These include rest, ice or heat therapy, and non-steroidal anti-inflammatory drugs (NSAIDs) to manage pain and inflammation. Physical therapy and stretching exercises can also help strengthen the muscles surrounding the piriformis and improve flexibility.
- Pain Management: In some cases, your doctor may prescribe muscle relaxants and pain medications or employ other pain management techniques to provide temporary relief from symptoms.
- Injections: If conservative measures do not provide sufficient relief, your healthcare provider may recommend injection therapies. These may include corticosteroid injections to reduce inflammation and alleviate pain.
- Surgical intervention: In rare cases where conservative treatments and injections have not been effective, surgical intervention may be necessary. This option is usually considered when there is significant compression of the sciatic nerve.
It is important to work closely with your orthopedic specialist to determine the most appropriate treatment plan for your specific condition.
Find Relief From Piriformis Syndrome at AOSMI in New Jersey
Understanding the symptoms, causes, and treatment options for Piriformis Syndrome is crucial for anyone experiencing this condition. Dr. Arth Patel and the team of orthopedic specialists at AOSMI are here to help you in your journey toward relief from piriformis syndrome.
Contact us to schedule an appointment with an orthopedic sports medicine doctor who can provide a comprehensive evaluation and develop an effective treatment plan tailored to your specific needs. Don’t let Piriformis Syndrome limit your mobility and quality of life any longer; take the first step towards relief by reaching out to AOSMI today.
Imagine a world where the simple act of walking doesn’t send jolts of pain through your body. Where every step isn’t a reminder of the relentless hip discomfort that’s been shadowing your every move. This isn’t a distant dream—it’s the reality that hip replacement surgery, or hip arthroplasty, promises. A beacon of hope for those tethered by hip pain and mobility challenges, this ground-breaking procedure is a game-changer, transforming lives by turning the tide on pain and unlocking a level of functionality many thought was lost forever. If you, or someone you hold dear, are on the brink of deciding on this life-altering surgery, journeying through the entire process, from contemplation to recovery, is essential. Let’s embark on this path together, uncovering the steps that lead from the shadows of discomfort to the light of renewed vitality.
Why Consider Hip Replacement Surgery?
Hip replacement becomes a consideration when alternative treatments, like medication, physical therapy, and lifestyle modifications, cease to alleviate pain or augment mobility. Common conditions warranting this surgery include osteoarthritis, rheumatoid arthritis, osteonecrosis, or injury-induced arthritis. The surgery aims to substitute the impaired hip joint parts with prosthetic components, thereby lessening pain and enhancing function. Notably, the choice of hip replacement type—such as traditional or minimally invasive, anterior or posterior approach, and the use of robotic assistance—can vary based on individual needs and the surgeon’s recommendation.

Preparing for Your Surgery
Medical Evaluation and Planning
A comprehensive evaluation by your orthopedic surgeon is critical before surgery. This step involves reviewing your medical history, performing physical examinations, and conducting imaging tests to devise a personalized surgical plan. According to the American Academy of Orthopaedic Surgeons, a detailed pre-operative evaluation is crucial for the success of hip replacement surgery.
Home and Lifestyle Preparations
Equally important is preparing your living space for post-surgery recovery. This might include securing assistance for daily tasks, making your home fall-proof, and setting up a main-level recovery area to avoid stair climbing initially.
Understanding the Surgical Process
The procedure entails removing damaged joint surfaces and replacing them with prosthetic parts made of metal, ceramic, and plastic. This transformation can significantly alleviate joint pain and restore mobility. Advancements in surgical techniques and anesthesia have made hip replacement a safe and effective option for many.
Navigating the Recovery Phase
Immediate Post-Surgery Care
Recovery promptly commences post-surgery, with most patients walking the same day of the procedure and often returning home shortly thereafter. This phase focuses on promptly managing pain and preventing complications.
Rehabilitation and Physical Activity
For the majority of patients, recovery from hip replacement surgery can be straightforward. The primary focus is on returning home and gradually increasing activity levels, primarily through walking. While some patients may benefit from additional physical therapy, it’s typically reserved for those experiencing difficulties, representing a minority—roughly 20%—of cases. Recovery and exercises can be tailored to individual needs, with the emphasis on self-guided progress.

Long-term Care and Activities
During the initial six weeks following surgery, patients should avoid impact activities such as running, jumping, or heavy lifting. After this period, assuming recovery progresses as expected, patients are encouraged to resume all activities, including returning to weight-lifting and sports based on their comfort level. Many individuals return to their usual daily routines within three months, with higher-intensity exercises or athletic activities typically resuming within three to six months.
Hip replacement surgery marks a significant milestone for those grappling with hip pain. We understand that this is a major surgery. We hope that by understanding the journey, from pre-surgery contemplation to recovery, you can improve your confidence and clarity regarding this decision. At AOSMI, our ultimate goal extends beyond pain relief. We hope to work with you to enhance your overall quality of life. We encourage you to engage in thorough discussions with our orthopedic surgeons so you can learn how hip replacement surgery can help you live a stronger and more active life. Request an appointment today to meet with our team of orthopedic surgeons to discuss if hip replacement surgery is right for you.
As Fall wraps us in its chilly embrace, you can bet basketball courts and ice skating rinks across New Jersey are buzzing with activity. Whether you’re part of a school team, hitting the court for a bit of fun, or gliding across the ice with friends and family, these Fall sports are a great way to stay active. With all the excitement, there’s also a chance of bumps, bruises, and sometimes more serious injuries. At AOSMI, we believe in patient education. We want to teach you about the more common Fall sports injuries, so that you are prepared and so that we can work together to get you back to your strongest self.
Common Fall Basketball Injuries:
Common Injuries: Some of the most common injuries in basketball are ankle sprains and anterior cruciate ligament (ACL) tears, both of which impact performance and long-term joint health.
Causes of Injury: Ankle sprains arise from the high-impact nature of basketball, particularly during rapid direction changes or awkward landings after jumps. ACL tears are often linked to abrupt stops, pivots, or sudden directional changes, exerting stress beyond the knee joint’s normal capacity.

Treatment and Surgery: Initial treatment for ankle sprains involves the R.I.C.E. protocol (Rest, Ice, Compression, and Elevation) to reduce swelling. ACL tears may necessitate surgical reconstruction using the patient’s tissues or grafts. At AOSMI, we are on the cutting-edge of orthopedic treatment – as such, we offer the BEAR (Bridge-Enhanced ACL Restoration) Implant that allows for natural healing without the need for grafts.
Physical Therapy Rehabilitation: Post-surgery, physical therapy becomes pivotal in restoring strength, flexibility, and joint stability. Progressive exercises targeting muscle strength, balance, and proprioception form the core of rehabilitation, guided by physical therapists to ensure a gradual return to play, minimizing the risk of re-injury. At AOSMI, our physical therapists tailor their treatment plans to your unique injury, ensuring a personalized approach.
Common Fall Ice Skating Injuries:
Common Injuries: Ice skaters frequently contend with fractures, particularly in vulnerable areas like the wrist and hip, because of the dynamic and sometimes acrobatic nature of the sport.
Causes of Injury: Falls on the ice, whether during jumps, spins, or routine skating, expose skaters to the risk of fractures. The hard frozen surface amplifies the impact, leading to fractures, especially in areas like the wrist and hip.

Treatment and Surgery: Immediate immobilization is important for managing fractures sustained during ice skating. Wrist fractures may require casting or splinting, while hip fractures may necessitate surgical intervention, involving plates, screws, or other fixation devices for proper alignment and stability.
Physical Therapy Rehabilitation: Rehab for ice skating injuries takes a comprehensive approach. Range-of-motion exercises are crucial for regaining flexibility, while progressive weight-bearing activities aid in rebuilding strength. Physical therapists craft tailored plans, integrating exercises that address the unique challenges of ice skating injuries, with a focus on enhancing balance, coordination, and functional movement. This personalized rehabilitation aims not only to restore functionality but also to prevent future injuries, facilitating a safe return to the ice.
By addressing the specific Fall sports injuries associated with basketball and ice skating, we aim to equip you with the knowledge needed to navigate the season safely. At AOSMI, our team is committed to providing the highest quality orthopedic and physical therapy care to our patients across New Jersey. If you are experiencing pain or injury from these sports, please request an appointment today. We are dedicated to helping you live a healthier, stronger life.
When it comes to hip replacement surgery, there are different approaches available, and each has its unique advantages and considerations. At Advanced Orthopedic and Sports Medicine Institute, Dr. Joseph Tauro and Dr. Eric Buxbaum specialize in Anterior Hip Replacement, a procedure that offers a minimally invasive approach with muscle preservation. Dr. Alan Nasar specializes in Posterior Hip Replacement, an established technique with a wide range of effective applications.
Hip Osteoarthritis

Hip replacement surgery is often recommended for individuals suffering from hip conditions, with osteoarthritis of the hip being one of the most common reasons. Hip osteoarthritis, a specific type of joint condition that affects the hip, often presents through distinctive symptoms. The most common and noticeable sign is hip pain, often felt deep in the hip, thigh, or groin, sometimes radiating to the knee and worsened by activities like walking. Stiffness in the hip, typically more pronounced in the morning or after inactivity, can make it challenging to start moving or stand up. Reduced range of motion affects your ability to perform everyday tasks, while a grating sensation may occur when you move your hip. Weakness in the muscles around the hip, swelling, tenderness, and joint deformities like bone spurs or alignment changes are additional telltale signs. If you’re experiencing these symptoms, we encourage you to reach out to the orthopedic specialists at AOSMI, for accurate diagnosis and effective management, especially since early intervention can alleviate pain, improve joint strength and function, and enhance your overall quality of life. Both anterior and posterior approaches can be used to address this condition effectively.
Anterior vs. Posterior Approach
1. Anterior Hip Replacement
The anterior approach is known for its minimally invasive features and muscle preservation. During this surgery, the incision is made at the front of the hip, allowing the surgeon to access the hip joint without cutting through major muscles. The minimally invasive nature of the procedure typically results in potentially faster recovery, reduced pain, shorter hospital stays, and improved mobility.
2. Posterior Hip Replacement
The posterior approach is a well-established and longstanding technique. It involves an incision at the back of the hip. The posterior approach is versatile and can effectively address a wide range of hip conditions. Surgeons often choose this approach due to their familiarity with it and the proven outcomes it offers. This approach may also be associated with potentially lower risk of nerve injury.
Choosing Between Anterior and Posterior Hip Replacement

The choice between anterior and posterior hip replacement surgery is a critical decision, and it should be based on a thorough evaluation of the patient’s individual case. Several factors come into play, including the patient’s anatomy, the surgeon’s expertise, and the specific surgical indications. Consulting with an experienced orthopedic surgeon is crucial in this process. They can assess your condition, consider these factors, and recommend the most suitable surgical approach for your specific needs. The success of your surgery is not solely dependent on the approach but also on the expertise of your surgeon and your commitment to post-operative rehabilitation.
If you’re experiencing any of the hip pain symptoms explained above or are considering hip replacement, please request an appointment today to consult with our experienced orthopedic surgeons. Let’s work together to manage your pain and get you back to your strongest self!
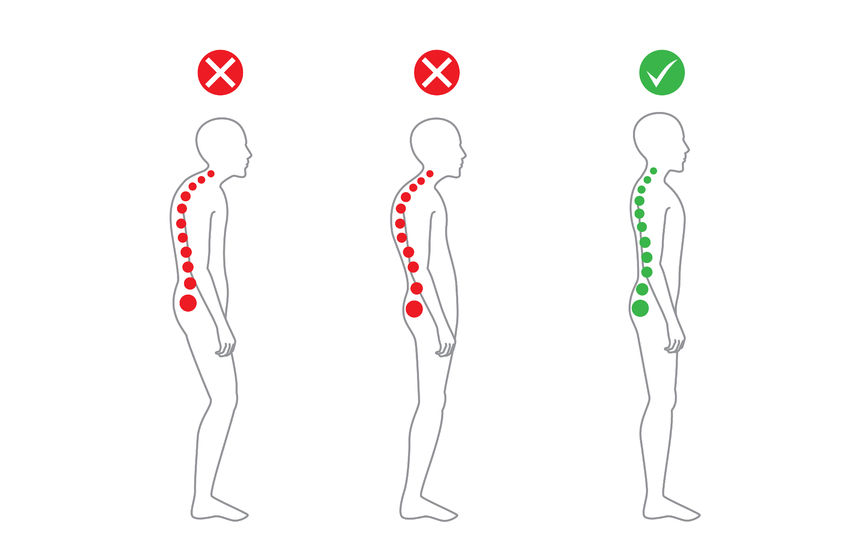
Poor posture has many detrimental effects on the body. Individuals often experience chronic pain in the back, neck, and shoulders, digestive issues, stiffness, and fatigue. Poor posture can also lead to nerve compression, muscle atrophy, carpal tunnel syndrome, and sciatica. Although sometimes unnoticed, posture also has a strong impact on the mind, considering people may experience worsened depression and stress, along with tension headaches.
Poor alignment creates ligament and muscle imbalances, which cause many problems. Deviations exist because of the imbalance of muscles, which work together in holding a joint in place. With one tight muscle and one loose one, muscles are pulled away from their rightful positions. Overactive muscles then overcompensate for underactive ones, causing issues and stress on the body.
There are various ways to improve posture, but it is important to understand exactly where alignment is impaired. To determine the postural deviation, one must conduct a standing assessment. During the assessment, which consists of various stances, the overactive and underactive muscles are assessed to discover the strengthening exercises that must be used.
To achieve an upright posture, individuals can follow a few simple steps.
- Step 1: Place feet shoulder width apart.
- Step 2: Stand up straight.
- Step 3: Keep weight on balls of feet.
- Step 4: Keep shoulders square.
- Step 5: Pull head back and up.
These steps can assist individuals who tend to hunch over from poor posture. The greatest challenge is to remain aware of your posture as you go about your day. It is easy to go minutes or hours without realized that you are slumping or slouching. One of the best ways to develop better posture is to be mindful of specific deviations and contact an orthopedic specialist for more assistance.

Millions of Americans suffer from from some degree of hip pain. You may have noticed a stiffness or discomfort in your hips in the morning, or experienced achiness or soreness after activities such as walking or jogging. This pain can be an early sign of hip arthritis.
To understand hip arthritis, you must understand how the hip joint works. The hip is a ball and socket joint and, similar to your shoulder, allows for a full range of movement. Both the ball and socket in the joint are covered with a layer of flexible cartilage to cushion the bones as you move. It is when this cartilage begins to wear down that you begin to experience painful symptoms of arthritis. As the cartilage continues to deteriorate, your body reacts by creating bone spurs within the joint. These small, bony growths inside the joint can cause you greater pain and lessen your mobility over time.
Depending on the severity of your condition, New Jersey orthopedic surgeons will develop a treatment plan which may include medication, physical therapy, and other supplemental treatments. However, when the joint cartilage wears away altogether, the bones in the hip socket rub together, resulting in nearly constant pain that can interrupt your daily routines. When hip arthritis symptoms are no longer manageable through medication, it is time to examine a surgical course of treatment. An orthopedic specialist may recommend minimally invasive hip replacement surgery to reduce your discomfort.
Many patients are concerned when their orthopedic specialist recommends hip replacement surgery. But this minimally invasive procedure is different than traditional hip replacement and offers many benefits.
The benefits of minimally invasive hip replacement surgery:
- Smaller incisions
- Less damage to surrounding muscles and bones
- Shorter hospital stay
- Quicker recovery
- Decreased risk of complications
- Less blood loss during surgery
Your team of NJ orthopedic specialists will develop the right course of treatment to meet your needs. To find out what your treatment options are, contact Advanced Orthopedics and Sports Medicine Institute to schedule an appointment.







