What’s New at AOSMI
We are thrilled to announce the partnership between Advanced Orthopedics and Sports Medicine Institute (AOSMI) and Joseph Tauro, MD and the former, Ocean County Sports Medicine! This collaboration is a significant milestone in our journey to enhance the quality of care and services we offer to our patients. By combining our strengths, we firmly believe we can reach new heights, offering improved services and advancing medical practices for the benefit of our patients, medical professionals, and the broader community.
Advanced Orthopedics and Sports Medicine Institute (AOSMI) is a leading provider of orthopedic care and sports medicine services in New Jersey, renowned for our commitment to delivering the highest quality care and ability to attract and retain top doctors in the industry. Our team consists of highly skilled orthopedic surgeons, physiatrists, physical therapists, and a multitude of musculoskeletal specialists dedicated to helping patients achieve their goals and regain an active lifestyle.
With this alliance, Ocean County Sports Medicine will undergo a name change, now joining the AOSMI brand name and growing the AOSMI network to 8 total locations across Monmouth, Ocean, Middlesex and Mercer counties.
This partnership will only further enhance the excellent care patients have come to expect from both groups. We remain committed to delivering the same high-quality care and personalized attention that patients have been accustomed to over the years, but now with greater resources and support.
In the coming months, you can look forward to the evolution of our partnership taking shape at our new Toms River facility as we transition in-office signage, our website, and beyond, to reflect all the improvements we are excited to bring to you. Our mission has always been to afford patients a personalized experience that focuses on the whole body, and through this transition, we are confident in our ability to continue delivering transformative outcomes in convenient ways.
So, how does this affect our existing Toms River location patients?
You can expect the same world-class service delivered by the same clinical staff.
We will now be participating in-network with several insurance plans including:
- Aetna
- Aetna Centre State
- Horizon
- Qualcare
- Medicare
Access to an expanded network of board-certified and fellowship-trained specialists within our network, including:
- General Orthopedics & Surgery
- Spine care
- Podiatry
- Pain management
- Physical medicine
- Physical therapy
- Sports medicine
You can look forward to an expanded geographic footprint, now serving 8 locations including: Toms River, Belmar, Brick, Edison, Freehold, Manalapan, Monroe and Robbinsville, NJ
Insurance Verification
For patients at our Toms River location, if you have insurance, we will verify and re-evaluate your insurance benefits under our AOSMI business name. Our goal is to provide the best, affordable care options for you.
New Practice Forms
For patients at our Toms River location, you will be asked to complete new office forms to acknowledge that your treatment will continue under the AOSMI name.
Correspondence Under our New Name
For patients that were treated with Ocean County Sports Medicine in the past, please keep an eye out for emails, texts or mail that may come with our new name: Advanced Orthopedic & Sports Medicine Institute. You will no longer receive communications from “Ocean County Sports Medicine”. If you should receive any correspondence from Ocean County Sports Medicine, please contact the office.
We would like to express our utmost gratitude for your continued trust and loyalty to AOSMI and Ocean County Sports Medicine. We are excited about the opportunities this partnership brings and look forward to providing you with exceptional care and improved services.
If you have any questions or would like further information about our partnership with AOSMI, please do not hesitate to reach out to our office. Our friendly staff is available to assist you.
Thank you for entrusting us with your orthopedic and sports medicine needs. We appreciate your ongoing support and look forward to serving you with the highest level of care.
Advanced Orthopedics and Sports Medicine Institute
 Anterior Cruciate Ligament (ACL) injuries are one of the most common knee injuries in the United States – approximately 400,000 ACL injuries occur every year. Historically, orthopedic surgeons have had limited options in treating a torn ACL. In ACL reconstruction, today’s standard of care, the surgeon completely removes the remaining torn ACL and reconstructs it with either a tendon from the patient’s own leg (called an autograft) or a deceased donor (called an allograft).
Anterior Cruciate Ligament (ACL) injuries are one of the most common knee injuries in the United States – approximately 400,000 ACL injuries occur every year. Historically, orthopedic surgeons have had limited options in treating a torn ACL. In ACL reconstruction, today’s standard of care, the surgeon completely removes the remaining torn ACL and reconstructs it with either a tendon from the patient’s own leg (called an autograft) or a deceased donor (called an allograft).
At Advanced Orthopedic Sports Medicine Institute (AOSMI), we are now offering a new technology called the BEAR® (Bridge-Enhanced ACL Restoration) Implant. The BEAR Implant is the first medical advancement granted approval from the U.S. Food and Drug Administration (FDA) that enables the body to heal its own torn ACL. This new approach is a paradigm shift from ACL reconstruction and is the first innovation in ACL tear treatment in more than 30 years.
AOSMI completed the first official procedure on November 15, 2022. Michael J. Greller, MD, MBA, CPE, FAAOS, a Board-Certified Orthopedic Surgeon who is Fellowship-trained in Sports Medicine led the procedure. He was assisted by Garret L. Sobol, MD, Board-Certified Orthopedic Surgeon who is also Fellowship-trained in Sports Medicine.
“There are a number of advantages to restoring a ligament instead of replacing it, and the BEAR Implant is an exciting medical technology that is the first to clinically demonstrate that it enables healing of the patient’s torn ACL while maintaining the natural knee anatomy,” said Dr. Greller “Encouraging clinical studies have shown faster recovery of muscle strength and higher patient satisfaction with regard to readiness to return to sport than traditional ACL reconstruction – the standard of care today.”
ACL Injuries – An Overview
Your knee joint is formed by three bones: the femur (thigh bone), tibia (shin bone), and patella (kneecap). The ACL (Anterior Cruciate Ligament) is one of the four main ligaments in the knee that helps to stabilize the joint. It is located in the center of the knee – it runs from the backside of the femur (thigh bone) to the front of the tibia (shin bone). The ACL is responsible for preventing the tibia from sliding out in front of the femur, and helping to control rotational movements of the knee.
The majority of ACL injuries are non-contact injuries – when athletes while running, rapidly change directions, stop or decelerate, or land from a jump without properly bending their knees. ACL injuries can also occur from direct contact to the knee joint. Most ACL injuries are complete tears, in which the ligament has been torn in half or pulled directly off the bone.
Patients usually report hearing and feeling a popping sensation during the injury. After the tear, patients experience pain with swelling, instability of the joint, loss of full range of motion, tenderness, and discomfort while walking.
ACL injury treatment is focused on preventing further knee instability and protecting the joint from further trauma. The two approaches to treatment are the non-surgical approach and the surgical approach. The approach is dependent on the extent of damage to the knee and the patient’s willingness to modify activity. Young and competitive athletes who want to return to activities that require aggressive jumping, cutting and pivoting or deceleration movements, and patients with meniscal tears usually pursue surgical reconstruction. Patients who have partial tears, do not have knee instability, and don’t partake in these “at-risk” movements can maintain their knee stability with physical therapy and rehabilitation alone. However, physical therapy is a core component of ACL treatment, surgical or non-surgical. For complete tears, surgery is usually recommended.
Standard ACL Reconstruction vs. BEAR Implant
ACL reconstruction surgery remains the gold standard of care. In this procedure, the surgeon takes tendon from the patient’s patellar tendon (patellar tendon autograft), hamstring tendon (hamstring tendon autograft), or from a human donor (allograft) to replace the torn ACL.
Unlike reconstruction, the BEAR Implant does not require a second surgical wound site to remove a healthy tendon from another part of the leg or the use of a donor tendon. The BEAR Implant acts as a bridge to help ends of the torn ACL heal together. The surgeon injects a small amount of the patient’s own blood into the implant and inserts it between the torn ends of the ACL in a minimally invasive procedure. The combination of the BEAR Implant and the patient’s blood enables the body to heal the torn ends of the ACL back together while maintaining the ACL’s original attachments to the femur and tibia. As the ACL heals, the BEAR Implant is reabsorbed by the body, within approximately eight weeks.
BEAR Implant – Clinical Evidence
Safety and effectiveness of the BEAR Implant is supported by clinical evidence. As shown in Murray et. al 2019, IKDC scores, a patient-completed tool which contains sections on knee symptoms, function, and sports activities, from the BEAR Implant procedure was similar to that of ACL reconstruction two years post-surgery. AP Laxity, which measures stability of the knee joint, is the same as ACL reconstruction two years post-surgery. The BEAR Implant provides statistically better hamstring strength at 6 and 12 months, with the trend sustained to 2 years. BEAR Implant patients were also more likely to experience fewer contralateral ACL tears (tears in the non-injured knee) at two years. MRI indicates that the BEAR implant facilitates healing of the native ACL so that its size, geometry, and tissue composition are more like native ACL tissue than autograft. 86 percent of BEAR patients returned to pivoting sports by one year.
Risks and Limitations of the BEAR Implant
Following the BEAR Implant, patients are directed to follow the BEAR Implant physical therapy program. The BEAR Implant has the same potential medical and surgical complications as other orthopedic surgical procedures, including ACL reconstruction. These include the risk of re-tear, infection, knee pain, meniscus injury and limited range of motion. The BEAR Implant is indicated for skeletally mature patients at least 14 years of age with a complete rupture of the ACL, as confirmed by MRI. Patients must have an ACL stump attached to the tibia to construct the repair. The BEAR device must be implanted within 50 days of injury.
If you meet these criteria, you may be a candidate for the BEAR Implant procedure. To learn more about the procedure, request an appointment. If you have questions about ACL tears or if you are experiencing knee pain, contact us. With offices across New Jersey, the physicians and staff of Advanced Orthopedic Sports Medicine Institute are committed to restoring your health so that you can get back to your active lifestyle as quickly and safely as possible. To learn more about how you can benefit from expert orthopedic treatment, call us (732.720.2555) or request an appointment today.

Michael C had a bilateral knee replacement done late February 2017 and only about 1 month after surgery, Michael is able to move better and is even doing a dance in honor of St. Patrick’s Day.
Here Michael is 6 weeks post bilateral knee replacement surgery, done late February 2017. Michael’s mobility is improving every day and is already to walk, run and dance a jig.
Dr. Greller specializes in advanced, minimally-invasive shoulder, knee, hip, and ankle arthroscopic procedures, including ACL, rotator cuff and meniscus surgery. He also performs minimally-invasive hip, knee and shoulder replacements. Dr. Greller, being on the cutting edge of technology in orthopedics, was one of the first New Jersey surgeons to do computer-assisted joint replacements in the tri-state area and he is always trained on the latest technologies to improve patient non-surgical and surgical outcomes.
See more of Dr. Greller’s testimonials.

As far as durable bones go in the hand, the knuckles are by far the most resilient, but even the strongest of knuckles are susceptible to bruising. There are 27 bones, and 29 joints in the human hand, but how can you tell if you’ve bruised any of these?
Have you ever suffered a direct hit to your hand? Accidentally walking by a table and smacking it with your hand? A fracture or bruise can occur when you incur a direct hit against a hard surface. Bruised knuckles are common injuries we see as orthopedic sports medicine professionals and are most frequently found in people who participate in mixed martial arts, boxing, and baseball activities. But anyone can bruise a knuckle. Below are the symptoms to look for if you think you may have bruised your knuckles:
- Sharp pain after impact
- Trouble making a fist
- Painful movement when opening and extending hand
- Swelling
- Stiffness after impact
Like all other injuries, the best route to decipher if your knuckles are bruised is to see a qualified orthopedic specialist for an accurate diagnosis and treatment plan. A splint may be issued to keep the knuckle in a proper position during the healing process. Anti-inflammatory medication may be prescribed; there are also natural anti-inflammatories that can be ingested, such as turmeric and curcumin supplements and teas.
If you feel like you have a bruised knuckle, it is suggested that you immediately visit an orthopedic specialist to treat injuries and enhance recovery.
A Doctor Gets A New Knee – How this physician handled his knee problem.
William Kohlberg, M.D.
For decades I stayed fit for tennis and skiing by speed walking on a treadmill. But towards the end of 2015 my right knee was giving me more and more pain. Finally I gave up the treadmill and started using the elliptical however the knee was getting worse. It got to a point where I would wake at night and have to walk around the house to help decrease the pain. Soon I was unable to play tennis. X-rays showed narrowing of the space between the femur (thigh bone) and tibia (lower leg bone) and an MRI showed loss of cartilage in the knee and bone marrow edema where the femur and tibia were hitting each other. Without the cartilage present to act as a cushion, bone was hitting bone. This caused pain not only during strenuous activity but also while walking, playing tennis, and even waking me up at night with pain that was unrelenting.
It was time to hit the textbooks and see what could be done. Weight loss was high on the list and after losing 20 pounds there was no improvement. Saw the orthopedist and got two shots of steroids and a shot of hyaluronic acid, which lubricates the knee. This helped for about 6 weeks but then the pain returned. An unloading brace did not help. This brace redirects the forces in the knee from the inside where the cartilage is deficient to the outside. I was considering a procedure that may help new cartilage grow. However, further medical literature search came up with articles that indicated that once bone marrow edema is present, such conservative measures will not work.
It was time to consider surgery. But where should I go? I checked out a large New Jersey institution but after checking out the “big” surgeons, I found out things I didn’t like. Same thing in New York City. I know how the system works. I trained in New York. There is nothing magic east of the Hudson. And really I wanted my surgery at CentraState anyway. I have worked at CentraState for 35 years and I know everything that goes on at CentraState. I know the surgeons, nurses, and technicians. I decided this is where I will get my surgery for there is no better place to have a knee replacement.
Dr. Alan Nasar does the most knee replacements at CentraState and Dr. Gregg Berkowitz the second most. I saw them both and they agreed to do a right “Uni” replacement, a surgery where the medial (towards the middle) knee joint is replaced. This is where the loss of cartilage was causing my problem. The lateral (towards the outside of the body) was not giving me a problem as it sustains less of a physical load then the medial.
As a surgeon, I wanted to watch my own surgery. The operating room has a video camera within the surgical lighting and the nursing staff set up a TV screen for me to watch. Anesthesia gave me a spinal and local nerve block, so I was fully awake and alert. The surgery was painless and uneventful. I even went home the same day.
When the anesthesia wore off, I took pain pills. Physical therapy came to the house and started mobilizing me immediately. The biggest problem was the post op pain that prevented sleep. I saw Dr. Mariam Ghobriel for pain management and with the medications she prescribed, there was marked improvement. After a week of physical therapy at home I continued PT at CentraState hospital. I was able to drive myself after one week.
Dan Eskes and Chris Lang were amazing as they pushed me to increase my range of motion and muscle strength. I was very motivated and also did my exercises at home. After three and one half weeks, I was back to work. Soon I was able to walk around the block without stopping. By 4 months I returned to playing tennis and at four and one half months not only could I ski, but I was also skiing the moguls (bumps) as if nothing was wrong with my knee.
I am extremely thankful to all involved with my knee replacement and highly recommend the total joint center at CentraState Medical Center and Advanced Orthopedics.

Figure 1.
a. Narrow disc space with the disc squeezed out medially
b. Bone marrow edema of the tibia
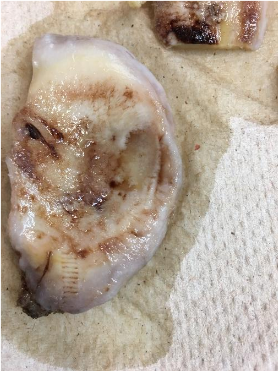
Figure 2. Tibial plateau with cartilage around the outside but loss of cartilage in the center.

Figure 3. Femoral condyle (knee side of the thigh bone) with loss of Cartilage in the middle.

Figure 4 Femoral Condyle articulating with tibial plateau.
Note how there is no cartilage in the middle from figures 2 and 3. This causes “bone on bone” pain.


Figure 5 & 6 Post operative x-rays. Metal cemented in place. The space between the two metal pieces is filled with a plastic disc (not visible on xray).

Figure 7. Beaver Creek, CO. Mogul run called “Moonshine”, 4 ½ months post op.
William Kohlberg, M.D.








