A Doctor Gets A New Knee – How this physician handled his knee problem.
William Kohlberg, M.D.
For decades I stayed fit for tennis and skiing by speed walking on a treadmill. But towards the end of 2015 my right knee was giving me more and more pain. Finally I gave up the treadmill and started using the elliptical however the knee was getting worse. It got to a point where I would wake at night and have to walk around the house to help decrease the pain. Soon I was unable to play tennis. X-rays showed narrowing of the space between the femur (thigh bone) and tibia (lower leg bone) and an MRI showed loss of cartilage in the knee and bone marrow edema where the femur and tibia were hitting each other. Without the cartilage present to act as a cushion, bone was hitting bone. This caused pain not only during strenuous activity but also while walking, playing tennis, and even waking me up at night with pain that was unrelenting.
It was time to hit the textbooks and see what could be done. Weight loss was high on the list and after losing 20 pounds there was no improvement. Saw the orthopedist and got two shots of steroids and a shot of hyaluronic acid, which lubricates the knee. This helped for about 6 weeks but then the pain returned. An unloading brace did not help. This brace redirects the forces in the knee from the inside where the cartilage is deficient to the outside. I was considering a procedure that may help new cartilage grow. However, further medical literature search came up with articles that indicated that once bone marrow edema is present, such conservative measures will not work.
It was time to consider surgery. But where should I go? I checked out a large New Jersey institution but after checking out the “big” surgeons, I found out things I didn’t like. Same thing in New York City. I know how the system works. I trained in New York. There is nothing magic east of the Hudson. And really I wanted my surgery at CentraState anyway. I have worked at CentraState for 35 years and I know everything that goes on at CentraState. I know the surgeons, nurses, and technicians. I decided this is where I will get my surgery for there is no better place to have a knee replacement.
Dr. Alan Nasar does the most knee replacements at CentraState and Dr. Gregg Berkowitz the second most. I saw them both and they agreed to do a right “Uni” replacement, a surgery where the medial (towards the middle) knee joint is replaced. This is where the loss of cartilage was causing my problem. The lateral (towards the outside of the body) was not giving me a problem as it sustains less of a physical load then the medial.
As a surgeon, I wanted to watch my own surgery. The operating room has a video camera within the surgical lighting and the nursing staff set up a TV screen for me to watch. Anesthesia gave me a spinal and local nerve block, so I was fully awake and alert. The surgery was painless and uneventful. I even went home the same day.
When the anesthesia wore off, I took pain pills. Physical therapy came to the house and started mobilizing me immediately. The biggest problem was the post op pain that prevented sleep. I saw Dr. Mariam Ghobriel for pain management and with the medications she prescribed, there was marked improvement. After a week of physical therapy at home I continued PT at CentraState hospital. I was able to drive myself after one week.
Dan Eskes and Chris Lang were amazing as they pushed me to increase my range of motion and muscle strength. I was very motivated and also did my exercises at home. After three and one half weeks, I was back to work. Soon I was able to walk around the block without stopping. By 4 months I returned to playing tennis and at four and one half months not only could I ski, but I was also skiing the moguls (bumps) as if nothing was wrong with my knee.
I am extremely thankful to all involved with my knee replacement and highly recommend the total joint center at CentraState Medical Center and Advanced Orthopedics.

Figure 1.
a. Narrow disc space with the disc squeezed out medially
b. Bone marrow edema of the tibia
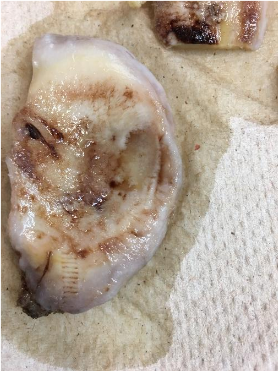
Figure 2. Tibial plateau with cartilage around the outside but loss of cartilage in the center.

Figure 3. Femoral condyle (knee side of the thigh bone) with loss of Cartilage in the middle.

Figure 4 Femoral Condyle articulating with tibial plateau.
Note how there is no cartilage in the middle from figures 2 and 3. This causes “bone on bone” pain.


Figure 5 & 6 Post operative x-rays. Metal cemented in place. The space between the two metal pieces is filled with a plastic disc (not visible on xray).

Figure 7. Beaver Creek, CO. Mogul run called “Moonshine”, 4 ½ months post op.
William Kohlberg, M.D.







